Lancet:意外发现几乎占据整个左心房的肿块,但患者一点症状也没有!——案例报道
2016-10-15 MedSci MedSci原创
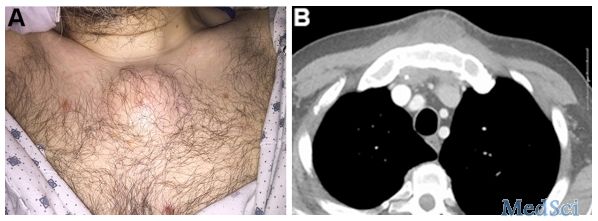
患者男,70岁,家庭医生进行常规检查时发现他有无症状的房颤,因此来医院进一步检查,经胸超声心动图发现一个大的房内肿块回声,几乎占据了整个左心房! 经食道超声心动图检查显示,占位性病变大小约9·5 × 7·2厘米,范围从房间隔、几乎占据整个左心房、膨胀到右心房,接近二尖瓣-主动脉连接处! 心脏MRI结果如下图,肿块混合纤维和囊性成分,周围有包裹。 冠状动脉造影正常,33
患者男,70岁,家庭医生进行常规检查时发现他有无症状的房颤,因此来医院进一步检查,经胸超声心动图发现一个大的房内肿块回声,几乎占据了整个左心房!
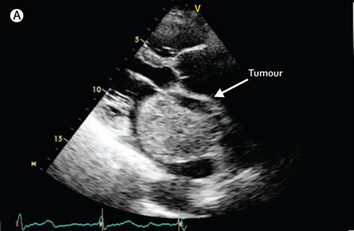
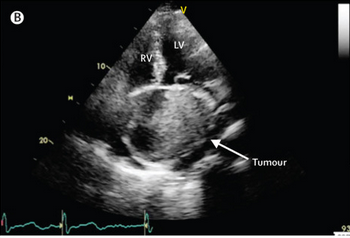
经食道超声心动图检查显示,占位性病变大小约9·5 × 7·2厘米,范围从房间隔、几乎占据整个左心房、膨胀到右心房,接近二尖瓣-主动脉连接处!
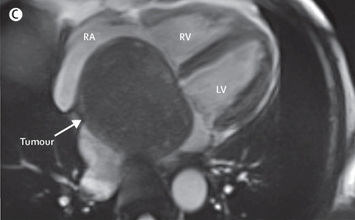
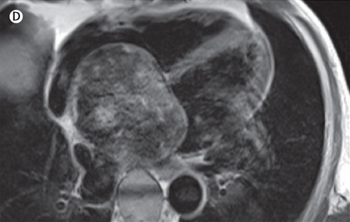
心脏MRI结果如下图,肿块混合纤维和囊性成分,周围有包裹。
冠状动脉造影正常,33FDG PET-CT没有发现FDG摄入增加。
经手术完全切除肿块,活检结果显示:血管肉瘤。
1年后,患者仍存在房颤,但是没有出现心脏或全身性肿瘤复发。
原发性心脏肿瘤是罕见的(占所有心脏肿瘤的0·0017–0·02%),其中肉瘤约占三分之一。30–45%的恶性肉瘤是血管肉瘤,通常出现在靠近房室沟的右心房(不像粘液瘤,它们很少出现从房间隔)。
患者的症状通常与肿瘤尺寸有关,如右心衰竭、挤压综合征、胸痛、心包积血等。心内型的预后一般都会很差,主要是因为它们往往呈现转移性疾病,最常见的肺和肝转移。
偶然发现血管肉瘤是十分罕见的!但对于心内肿瘤的评价是复杂的。超声心动图可以很好的评估肿瘤的血流动力学,心脏磁共振则有利于发现肿瘤浸润和组织特征。
原始出处:
Alfonso Campanile,et al.An unexpected finding in an asymptomatic patient with atrial fibrillation: cardiac angiosarcoma.Lancet.11 June 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#左心房#
34
#Lancet#
30
#肿块#
24
#心房#
26
好好学习
71
很好,不错,以后会多学习
57
很罕见的病!
58
这个案例挺不错的!
61
继续关注
63
谢谢指点迷津学习了
27