胰头肿块一例-----放射科病例讨论(复旦大学附属中山医院)
2015-12-10 武丽芳 曾蒙苏 复旦大学附属中山医院放射科
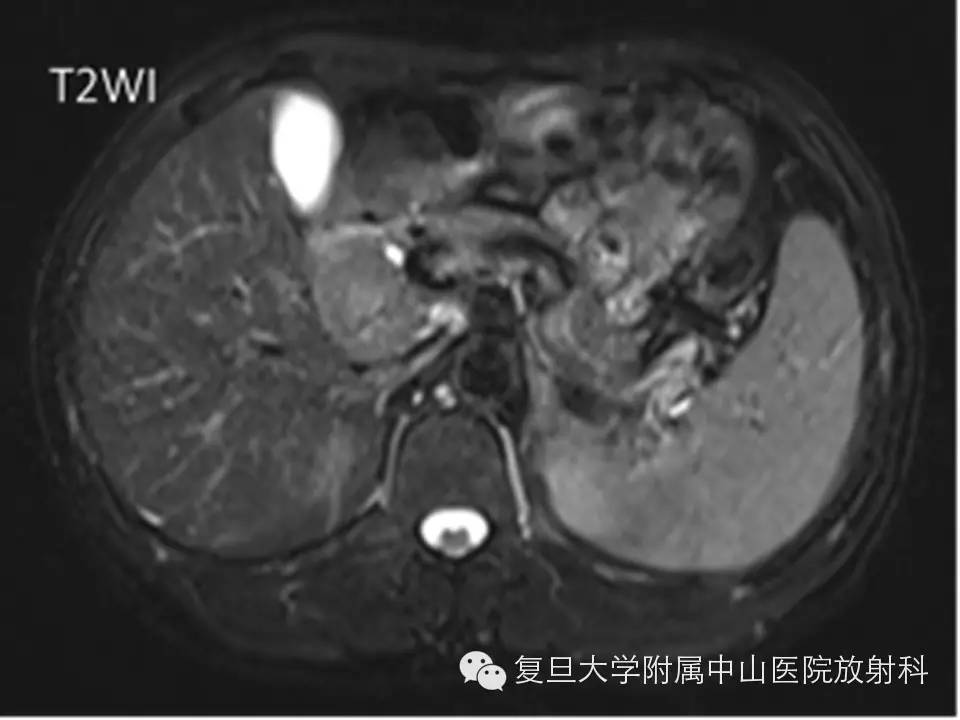
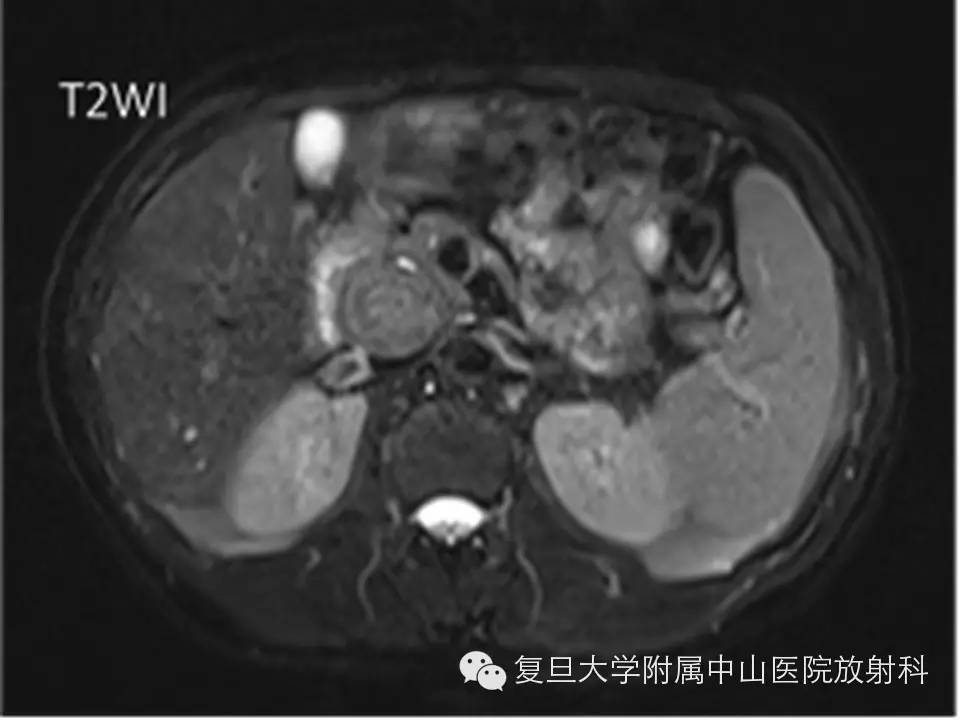
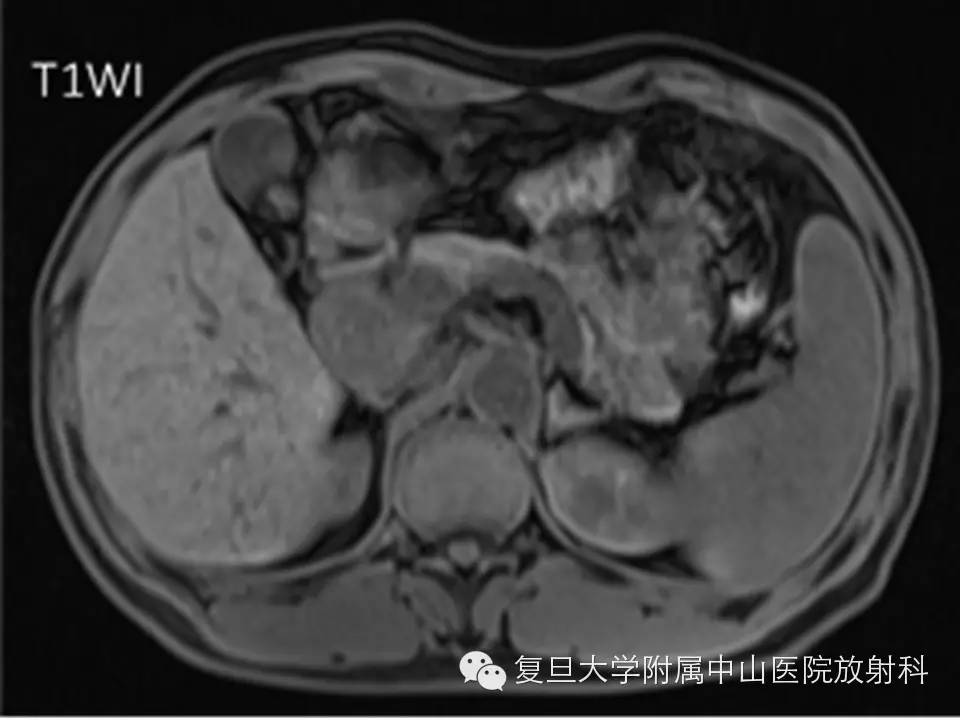
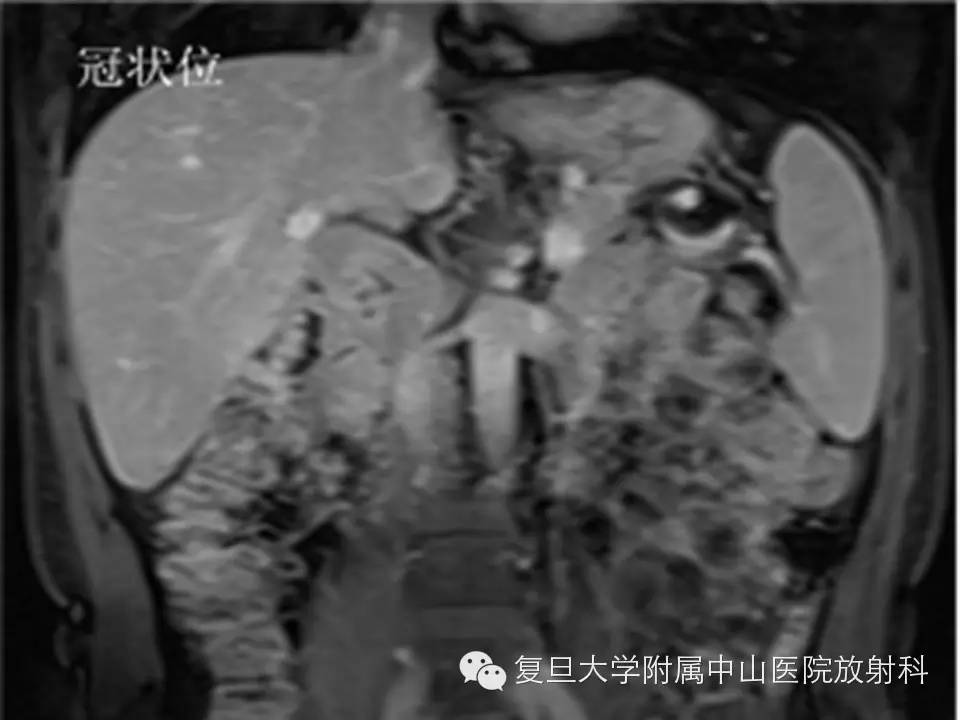
病史 男性,54岁,超声体检发现胰头肿块,临床症状和实验室检查阴性。 【CT】 【MRI】 答案往下 影像学表现 CT平扫可见胰头区一软组织肿块,密度不均,中央为斑片状低密度;MRI表现为T2不均匀稍高信号,T1低信号,增强扫描动脉期较明显强化,门脉期及延迟期逐渐填充,冠状位显示两相邻肿块(下方者略小),未






答案往下
{nextpage}
影像学表现
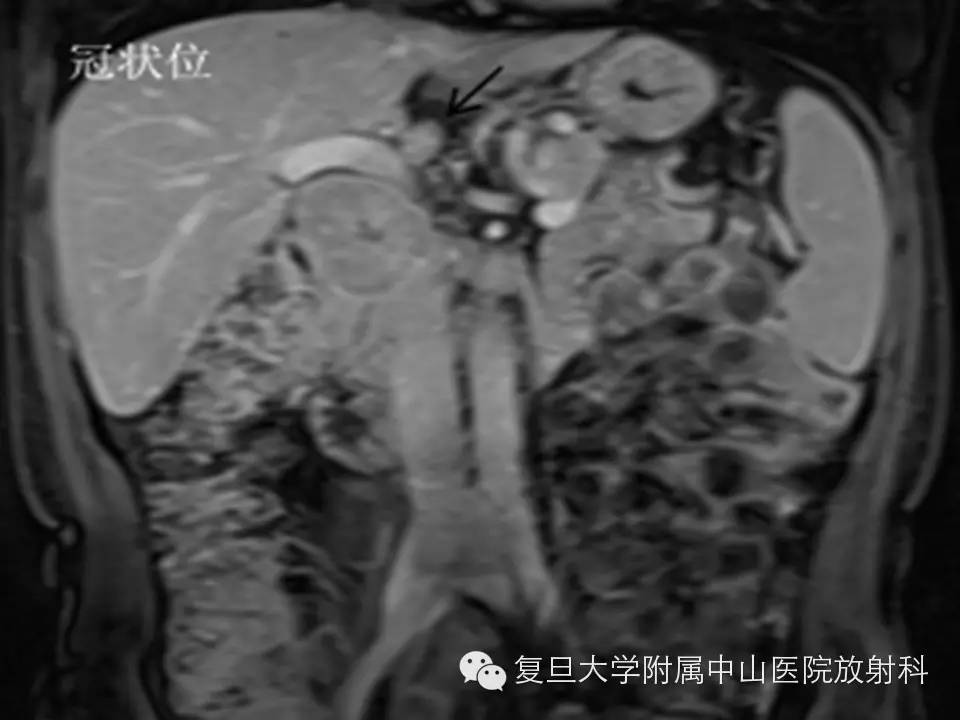
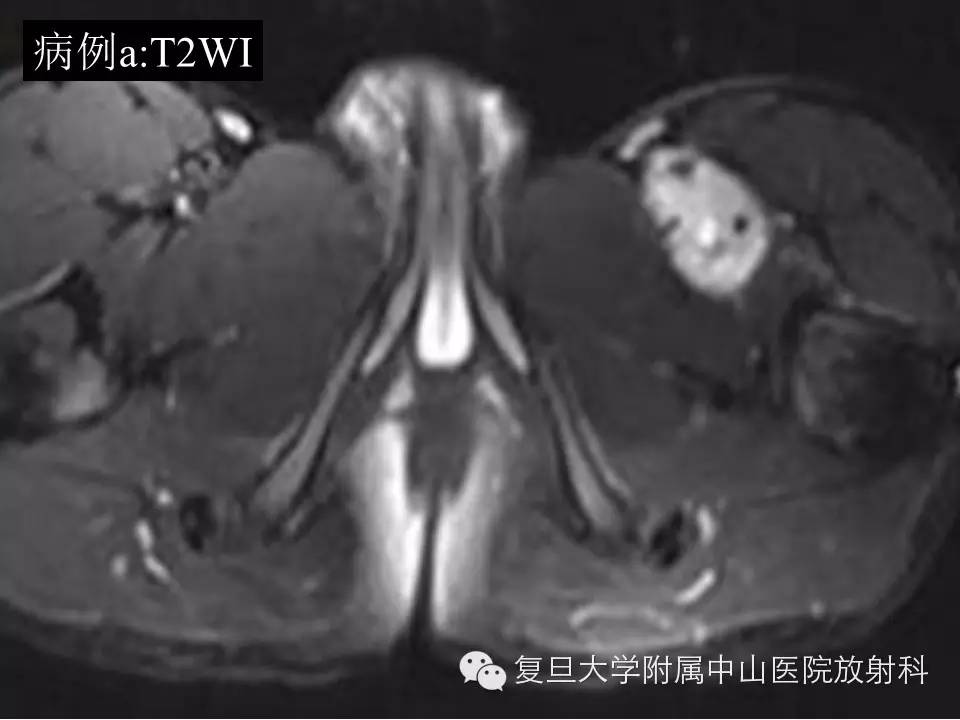
CT平扫可见胰头区一软组织肿块,密度不均,中央为斑片状低密度;MRI表现为T2不均匀稍高信号,T1低信号,增强扫描动脉期较明显强化,门脉期及延迟期逐渐填充,冠状位显示两相邻肿块(下方者略小),未见胰管扩张,与门静脉关系密切,门脉旁见稍大淋巴结。
手术病理结果
巨检:
剖开十二指肠及胰腺组织,见灰白色肿物两枚,大者约5X3X3CM,小者直径为3CM,切面灰白色,质中等,周围界尚清。
诊断:
(胰十二指肠)神经内分泌癌(细胞形态相当于现行WHO分级,II级),检出胰头淋巴结5枚,其中1枚见癌转移(1/5)。
免疫组化:
Calcitonin(-),SYN(60%+),CHG(100%++),CD56(15%+),KI67(5%++),inSulin(-),Glucogen(-),PP(部分+),ACT(-),Soma(-),Serotonin(-),VIP(-),NSE(-),a-AT(-).
讨论
WHO 2010指南将胰腺神经内分泌肿瘤(pancreatic neuroendocrine tumors, PNETs)分成三级:低级别神经内分泌肿瘤(G1,Ki-67指数<3%,分化程度较高),中级别神经内分泌肿瘤(G2,3%≤Ki-67指数≤20%,中等分化),高级别神经内分泌瘤(G3, Ki-67指数>20%,分化程度差)。胰腺神经内分泌癌约占胰腺恶性肿瘤的5%,男女发病率相当,多见于50-60岁患者。胰头区富血供肿瘤或肿瘤样病变除了胰腺来源的 神经内分泌肿瘤,还包括十二指肠间质瘤、异位嗜铬细胞瘤、和巨淋巴增生症等。鉴别关键肿瘤定位,如来源胰头者,常可见肿瘤与正常胰腺呈“喇叭口”样改变;而非胰腺起源者,胰腺组织常被推移或与胰腺境界不清。鉴别关键定位,即来源胰头者,常可见肿瘤与正常胰腺呈“喇叭口”样改变。
PNET分为功能性和非功能性两类,前者根据分泌的激素种类分为胰岛素瘤、胃泌素瘤、胰高血糖素瘤、血管活性肠肽瘤(VIP瘤) 和生长抑素瘤等;后者占PNET 15-25%,常因肿瘤较大引起压迫症状时被发现,包括腹痛、梗阻性黄疸、肠道出血等。非功能性PNET大小与其潜在恶性度有关,<2cm者通常为良性,恶性者可见肝血管旁淋巴结转移。典型的PNET影像学表现为:边界常较规则,实性多见,动脉期较明显强化并持续强化;由于出血或坏死出现囊性变,囊变者多为单房,与周围胰腺实质以纤维包膜相隔,肿块沿胰腺导管生长时引起胰管扩张。
鉴别诊断:实性者需与胰腺癌(胰腺癌常血管包绕,引起胰胆管扩张,远端胰腺实质的萎缩,临床化验CA19-9等肿瘤标志物升高);实性假乳头状瘤(好发于年轻女性,胰尾多见,可囊变,轻度强化及延迟强化)鉴别;囊性者需与浆液性/粘液性囊腺瘤、导管内乳头状粘液性肿瘤及假性囊肿鉴别。
参考文献
[1] Bosman F, Cameiro FHruban R, et al. WHO Classification of Tumours of the Digestive System [M]. Lyon,France: IARC Press, 2010.
[2] Sarmiento JM, Farnell MB, Que FG, Nagorney DM. Pancreaticoduodenectomy for islet cell tumors of the head of the pancreas: long-term survival analysis. World J Surg 2002; 26:1267-1271.
[3] Graziani R, Brandalise A, Bellotti M, et al. Imaging of neuroendocrine gastroenteropancreatic tumours. Radiol Med 2010; 115:1047-1064.
[4]Vassos N, Agaimy A, Klein P, Hohenberger W, Croner RS. Solid-pseudopapillary neoplasm (SPN) of the pancreas: case series and literature review on an enigmatic entity. Int J Clin Exp Pathol 2013; 6:1051-1059.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#病例讨论#
43
#放射科#
42
很值得学习
102
好文章,值得看。
55
好文章,值得看。
93
…………
81
#肿块#
41
#中山医院#
44
#复旦#
39