Stroke:血压水平是否影响动脉内治疗的安全性?
2017-04-25 MedSci MedSci原创
高血压(BP)与不良结局和急性缺血性脑卒中并发颅内出血有关。但是,BP是否影响动脉内治疗(IAT)的安全性及益处尚不清楚。近期,一项发表在杂志Stroke上的研究旨在评估BP与功能结局、颅内出血症状和IAT的作用之间的关系。此项研究是MR CLEAN(荷兰急性缺血性卒中血管内治疗多中心随机临床试验)的析因分析。在基线、IAT或中风入院之前测量血压。估计基线BP与90天改良Rankin量表评分的关系
高血压(BP)与不良结局和急性缺血性脑卒中并发颅内出血有关。但是,BP是否影响动脉内治疗(IAT)的安全性及益处尚不清楚。
近期,一项发表在杂志Stroke上的研究旨在评估BP与功能结局、颅内出血症状和IAT的作用之间的关系。
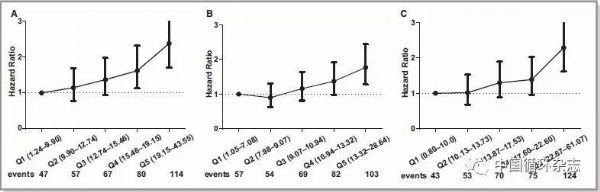
此项研究是MR CLEAN(荷兰急性缺血性卒中血管内治疗多中心随机临床试验)的析因分析。在基线、IAT或中风入院之前测量血压。估计基线BP与90天改良Rankin量表评分的关系,以及顺序和逻辑回归分析的安全参数。使用乘法相互作用项测试BP对IAT作用的影响。
此项研究结果显示:收缩压(SBP)与功能结局有最佳的相关性。这种相关性为U形;低基线和高基线SBP与功能不良结果相关。更高的SBP与颅内出血症状相关(调整的优势比,每10mm Hg高的SBP[95%置信区间,1.09-1.44]为1.25)。在SBP和IAT之间,功能结果、颅内出血症状或其他安全性参数之间没有相互作用;对于整个SBP范围,IAT的绝对优势是显而易见的。对舒张压的研究也有同样的发现。
此项研究表明:在由近端颅内血管阻塞引起的急性缺血性卒中患者中,BP不会影响IAT的益处或安全性。不应该因为BP而拒绝或延迟IAT。
原始出处:
Mulder MJHL, Ergezen S, et al. Baseline Blood Pressure Effect on the Benefit and Safety of Intra-Arterial Treatment in MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke in the Netherlands). Stroke. 2017 Apr 21. pii: STROKEAHA.116.016225. doi: 10.1161/STROKEAHA.116.016225.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血压水平#
0
文章很好,值得读
43
文章不错,值得分享
33
学习了分享了
49
学习一下
55