NEJM:阑尾蛲虫病-病例报道
2018-03-29 xing.T MedSci原创
蛲虫,众所周知,是一种线虫,最常见于儿童,尽管成年人也可感染。妊娠雌性蛲虫粘附于盲肠附近组织,并且迁移到肛门部位产卵,可引起肛周瘙痒症。通过接触被虫卵污染的手、浴室、床上用品、食品和其他来源进行自体感染和传播。很难确定存在患者阑尾内的蛲虫是引起患者症状的原因,还是一个偶然的发现。
患者为一名45岁的男性,因腹痛和没有食欲1天而到急诊就诊,该患者没有发热。
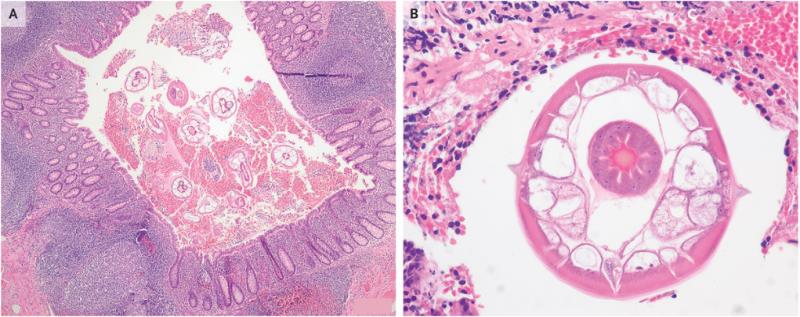
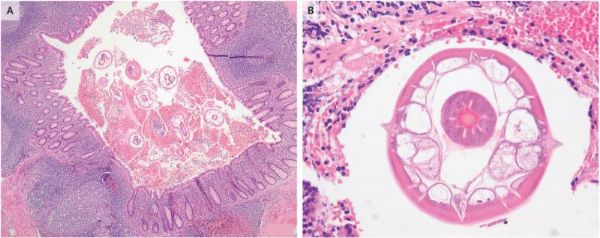
体格检查显示右下腹有压痛、反弹痛,Blumberg征阴性。实验室检查结果包括正常的白细胞计数,中性粒细胞占82%。腹部超声检查结果不确定有无阑尾发炎。该患者接受阑尾切除术。阑尾大体正常,但病理分析发现阑尾腔内存在蛲虫(图A和B,苏木精伊红染色)和黏膜轻度炎症。
蛲虫,众所周知,是一种线虫,最常见于儿童,尽管成年人也可感染。妊娠雌性蛲虫粘附于盲肠附近组织,并且迁移到肛门部位产卵,可引起肛周瘙痒症。通过接触被虫卵污染的手、浴室、床上用品、食品和其他来源进行自体感染和传播。很难确定存在患者阑尾内的蛲虫是引起患者症状的原因,还是一个偶然的发现。
该患者阑尾切除术后,患者和家属均服用甲苯咪唑。术后随访6个月,患者症状无复发。
原始出处:
Ismael Mora-Guzmán,et al. Appendiceal Pinworms.N Engl J Med 2018. http://www.nejm.org/doi/full/10.1056/NEJMicm1713306
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










一起学习学习
73
学习
59
学习
72
学习了
71
了解了解.继续关注
58