Alz Res Therapy:新型脑脊液蛋白,可有效区分痴呆和认知减退
2021-11-08 Freeman MedSci原创
N-224 tau可以区分AD受试者和SCD,并且可以区分非AD痴呆症的亚组和AD。
Tau病理学,以高磷酸化tau的神经纤维缠结(NFT)的形式,与淀粉样β(Aβ)斑块一起,是阿尔茨海默病(AD)的标志之一。Tau蛋白可在脑脊液(CSF)中被测量为总tau(T-tau),在AD和其他神经系统疾病中增加,并作为磷酸化tau(P-tau181),在AD中增加明显。
另一方面,Aβ42显示CSF水平下降。这些变化发生在临床症状发生前几十年,Aβ42的变化首先出现,其次是P-tau181和T-tau。这些蛋白通常通过免疫测定法(酶联免疫吸附法,ELISA)在CSF中测量。特别是传统的tau免疫测定,针对的是蛋白质的中间区域(T-tau)或单一的磷酸化位点(Thr181)。
然而,一些研究表明,CSF中的tau是非常异质的,它不是以全长蛋白的形式存在,而是以一系列片段的形式存在,主要属于蛋白的N端和中间区域,而不是C端。
在最近的一项研究中,瑞典隆德大学的Kaj等人观察到CSF中相对丰富的tau种类在氨基酸(aa)224处结束,可以用超灵敏的免疫测定法(单分子阵列,Simoa)测量。与健康的老年对照组或其他神经系统疾病的受试者相比,这些横跨Aa 224(N-224)的tau片段在AD受试者的CSF中明显更丰富。这些片段的CSF浓度与原发性tau病如进行性核上麻痹(PSP)和皮质基底综合征(CBS)中的T-tau浓度不相关,表明在这些疾病中量化N-224有助于与AD的鉴别诊断,因为经典的tau生物标志物在非AD痴呆症中通常是正常的。总之,这些结果表明,N-224的增加是AD的特异性,Kaj等希望在独立的队列中验证这些发现,包括认知健康的受试者和与AD无关的认知障碍患者。
转诊到记忆诊所的病人最初往往被诊断为主观认知能力下降(SCD)。SCD被定义为未被客观认知测试证实的自我感知的认知衰退。目前还不清楚SCD和早期AD之间存在哪种关系,以及有多大比例的SCD患者会发展成MCI或痴呆。即使没有客观的认知障碍证据,这些人中至少有一部分人的认知能力下降的风险增加;同时,他们也可能最终不会出现认知能力下降的进一步发展或演变为明显的AD。在早期阶段对SCD和AD或其他痴呆症的鉴别诊断是有问题的:对SCD的CSF Aβ42、T-tau和P-tau181水平的研究显示结果不一,没有对SCD患者CSF tau片段的研究。
藉此,隆德大学的Claudia Cicognola1等人在一个多中心研究中对N-224 tau检测进行临床验证,有两个独立的队列,一个包括SCD和可能的AD(队列1),一个包括认知健康的对照组、SCD、轻度认知障碍(MCI)、AD和非AD痴呆症患者(队列2)。
该研究包括来自阿姆斯特丹痴呆症队列的30个SCD和30个可能的AD(队列1)和来自瑞典BioFINDER研究(队列2)的539个对照,其中195个SCD,232个MCI,137个AD和253个非AD。所有样本都有AD核心生物标志物(Aβ42、T-tau、P-tau181)的测量。N-224是用超灵敏的Simoa检测法测量的。
与SCD相比,AD的N-224水平明显较高(队列1:p = 0.003),与队列2的所有其他诊断组(对照组、SCD、MCI和非AD,p < 0.0001)相比,AD的N-224也明显较高。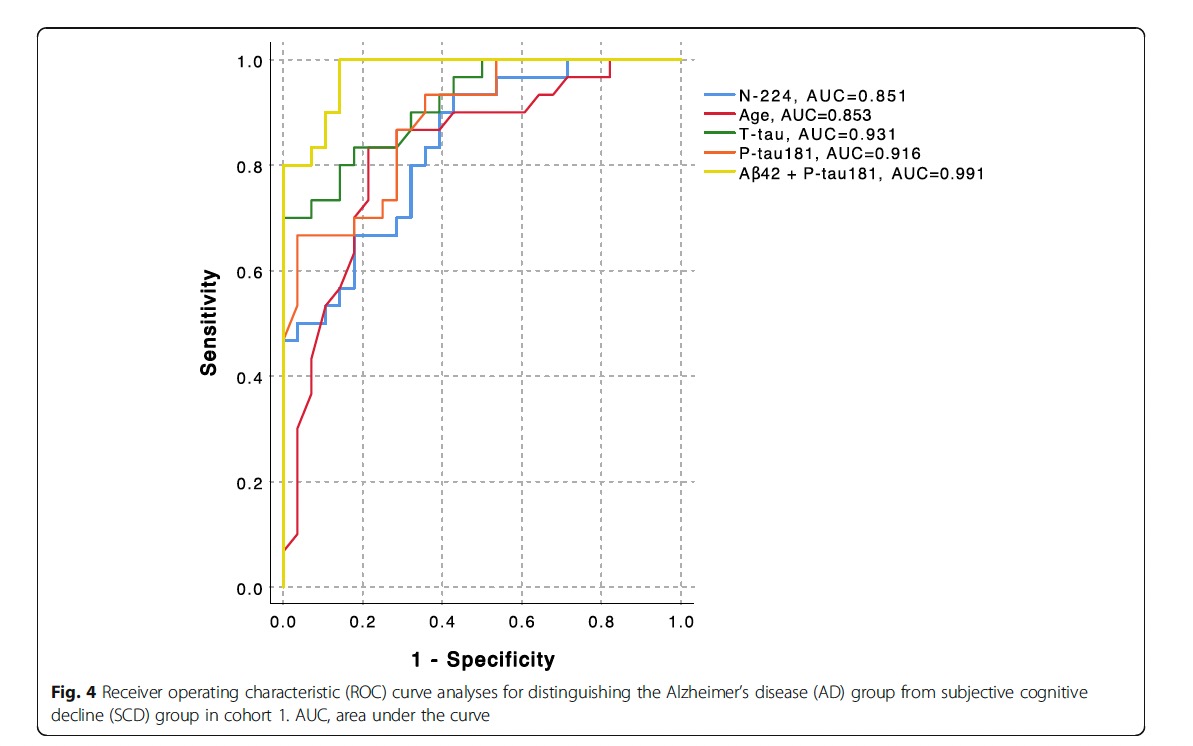
在非AD组中,N-224在帕金森病(PD,p < 0.0001)、帕金森病痴呆(PDD,p = 0.004)、进行性核上麻痹(PSP,< 0.0001)、多系统萎缩(MSA,p = 0.002)和未指明的帕金森病(NOS,p = 0.007)中显示的浓度明显低于AD。在队列1中,较高浓度的N-224与较低的迷你精神状态检查(MMSE)得分有关(R2 = 0.318,β = 0.564,p ≤ 0.0001),并能准确识别病态(<24)MMSE得分(p < 0.0001,AUC = 0.824)。
该研究的重要意义在于发现了:N-224 tau可以区分AD受试者和SCD,并且可以区分非AD痴呆症的亚组和AD。
原文出处:
Cicognola C, Hansson O, Scheltens P, et al. Cerebrospinal fluid N-224 tau helps discriminate Alzheimer’s disease from subjective cognitive decline and other dementias. Alz Res Therapy. 2021;13(1):38. doi:10.1186/s13195-020-00756-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#ERA#
35
#认知减退#
35
项研究旨在评估晚期肝纤维化非酒精
59
学习了
0
认真学习了
0
很好的参考
57
!n
48
有帮助
32
学习了,谢谢分享
32
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
21