Clin Gastroenterol H:基于人群的成人溃疡性结肠炎自然病史分析!
2017-06-18 xing.T MedSci原创
随着时间推移,UC是一种致残性疾病。需要进行前瞻性队列研究来评估疾病修饰疗法早期使用、治疗目标的方法、免疫调节剂和生物制剂等新策略的影响。也还需要从低发病地区进行长期研究。
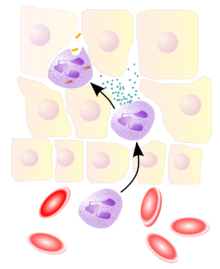
全面了解溃疡性结肠炎(UC)的自然病史有助于了解疾病的演变,识别不良预后指标以及对治疗策略的影响,并且促进共同决策。近日,消化病领域权威杂志Clinical Gastroenterology and Hepatology发表了一篇荟萃分析文章,研究人员系统地回顾了长期随访的以成年人群为基础的队列研究中UC的自然病史。
研究通过系统地检索了MEDLINE,截止日期到2016年3月31日,研究人员确定了在17个以人群为基础的起始队列中完成的60项研究,这些研究报告了成人发病UC(n=15316例UC患者)患者的长期病程和结局。
研究人员发现左侧结肠炎是UC最常见的部位,在10%至30%的病人中观察到疾病的扩展。大多数患者有轻度至中度的病程,在诊断时最为活跃,然后在不同的缓解期或轻度活动期有所变化,约10-15%的患者经历了一个积极的病程,10年累积复发风险为70%-80%。几乎50%的病人需要UC相关的住院,5年再住院的风险约为50%。5、10年结肠切除的累积风险为10-15%;达到黏膜愈合与较低的结肠切除风险相关。约50%的患者接受了糖皮质激素治疗,虽然这一比例随着时间已经有所降低,免疫调节剂(20%)和抗肿瘤坏死因子(5-10%)的使用相应的有所增加。虽然UC与死亡风险增加无关,但它与高发病率和工作残疾有关,相比于Crohn病。
随着时间推移,UC是一种致残性疾病。需要进行前瞻性队列研究来评估疾病修饰疗法早期使用、治疗目标的方法、免疫调节剂和生物制剂等新策略的影响。也还需要从低发病地区进行长期研究。
原始出处:
Mathurin Fumery,et al. Natural History of Adult Ulcerative Colitis in Population-based Cohorts: A Systematic Review. Clinical gastroenterology and hepatology 2017. http://www.cghjournal.org/article/S1542-3565(17)30722-X/fulltext
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#溃疡性#
36
#GAS#
22
#AST#
35
#Gastroenterol#
25
学习了谢谢分享!!!
49
学习了谢谢分享。
48
学习了谢谢分享!!
55
学习了
50
学习了,谢谢作者分享!
43