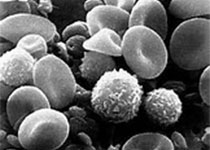
Blood:P4HA2通过羟基化Carbin促进B细胞淋巴瘤进展
2018-02-04 MedSci MedSci原创
中心点:P4HA2与DLBCL患者的病程进展和总体存活率差相关,可作为新的生物标志物和治疗靶点。P4HA2通过对Carabin的Pro306位点羟基化来抵消Carabin对淋巴瘤的负性作用。摘要:B细胞淋巴瘤是一种异质性的血液病,可选择的治疗方式有限,容易复发或进展成难治性。Carabin,B细胞受体信号和增殖的一种关键抑制剂,在B细胞淋巴瘤中处于失活状态,而且其机制不明。研究人员发现P4HA2(
中心点:
P4HA2与DLBCL患者的病程进展和总体存活率差相关,可作为新的生物标志物和治疗靶点。
P4HA2通过对Carabin的Pro306位点羟基化来抵消Carabin对淋巴瘤的负性作用。
摘要:
B细胞淋巴瘤是一种异质性的血液病,可选择的治疗方式有限,容易复发或进展成难治性。Carabin,B细胞受体信号和增殖的一种关键抑制剂,在B细胞淋巴瘤中处于失活状态,而且其机制不明。
研究人员发现P4HA2(脯氨酰4-羟化酶2)是Carabin的一种特异性的脯氨酸羟化酶。Carabin羟基化会导致其蛋白酶体降解,从而激活Ras/ERK通路,增加B细胞淋巴瘤增殖。P4HA2在正常的B细胞中检测不到,但在弥漫性大B细胞淋巴瘤(DLBCL)中上调,使Carabin失活、促进淋巴瘤增殖。
本研究结果表明P4HA2是DLBCL的一种潜在的预后标志,是一种有前景的药物靶点,可用来治疗分子层次的B细胞淋巴瘤。
原始出处:
Wei Jiang,et al.Prolyl 4-Hydroxylase 2 Promotes B-cell Lymphoma Progression via Hydroxylation of Carabin.Blood 2018 :blood-2017-07-794875; doi: https://doi.org/10.1182/blood-2017-07-794875
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞淋巴瘤#
23
#羟基化#
40
#P4HA2#
42
学习了谢谢分享!!
61
学习了感谢分享
55
#B细胞#
32