CLIN CANCER RES:结直肠腺瘤的循环标志物
2018-05-16 MedSci MedSci原创
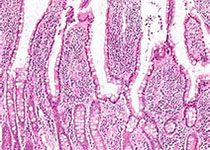
结直肠癌是世界范围内发病率第三的肿瘤,每年会导致700000人死亡。大部分结直肠癌良性时为腺瘤。结直肠腺瘤的检测目前往往由结肠镜完成,但是由于其较高的成本及侵入性,该检查通常局限于有家族史等高风险人群。CLIN CANCER RES近期发表了一篇文章,娅就是否可以用血液里的小RNA标志检测结直肠腺瘤。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
27
#结直肠#
19
学习了谢谢
61
学习了.谢谢分享
50