Circulation:B型主动脉夹层治疗:如何选择?
2015-09-30 张旭栋 MedSci原创
休斯敦德克萨斯大学医学院Afifi RO等人研究了B型主动脉夹层患者的远期结局,成果发表在8月份Circulation期刊上。背景:主动脉夹层(Aortic Dissection,AD)是最主要的主动脉上的灾难性疾病。在血管腔内时代,急性B型主动脉夹层(acute type B aortic dissection, ATBAD)的治疗最引入注目。本项研究旨在评估我们中心治疗时间已经超过13年ATB
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
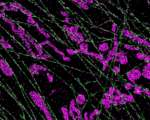








#B型主动脉夹层#
28
#主动脉#
23
#动脉夹层#
34