DCR: 克罗恩病患者回结肠切除术后 1 个月行内镜评估可预测未来术后复发情况
2022-03-15 MedSci原创 MedSci原创
肠镜是一支细长可弯曲的医学仪器,直径大约1厘米,结肠镜通过肛门进入直肠,直到大肠,可让医生观察到结肠和大肠的内部情况。结肠镜检查是医生用来检查大肠及结肠内部病变的一种诊断方式。
克罗恩病(CD)是一种慢性的破坏性肠道疾病,近50%的患者在患病头十年内需要进行肠道切除。手术对CD来说不是治愈性的,而且术后复发是很常见的。由于早期的CD术后内镜评估和及时的治疗调整是减少临床或手术复发风险的关键,内镜检查被推荐为确定术后复发的金标准。指南推荐所有患者在术后6-12个月进行内镜检查。然而,内窥镜复发的发生率在一年内可高达70-90%,因此,早期的术后内窥镜监测可能有助于在早期阶段对治疗进行调整。因此,本项研究旨在确定术后 1 个月内镜评估的特征、临床价值和安全性。

为此,研究人员进行了一项前瞻性观察研究,作者将 2016 年 1 月至 2018 年 11 月期间接受回结肠切除术的克罗恩病患者纳入了研究分析。所有患者的第一次术后回结肠镜检查在术后 4-5 周进行。主要观察结果是术后12 个月内的术后复发,最后进行单变量和多变量分析以确定风险因素。
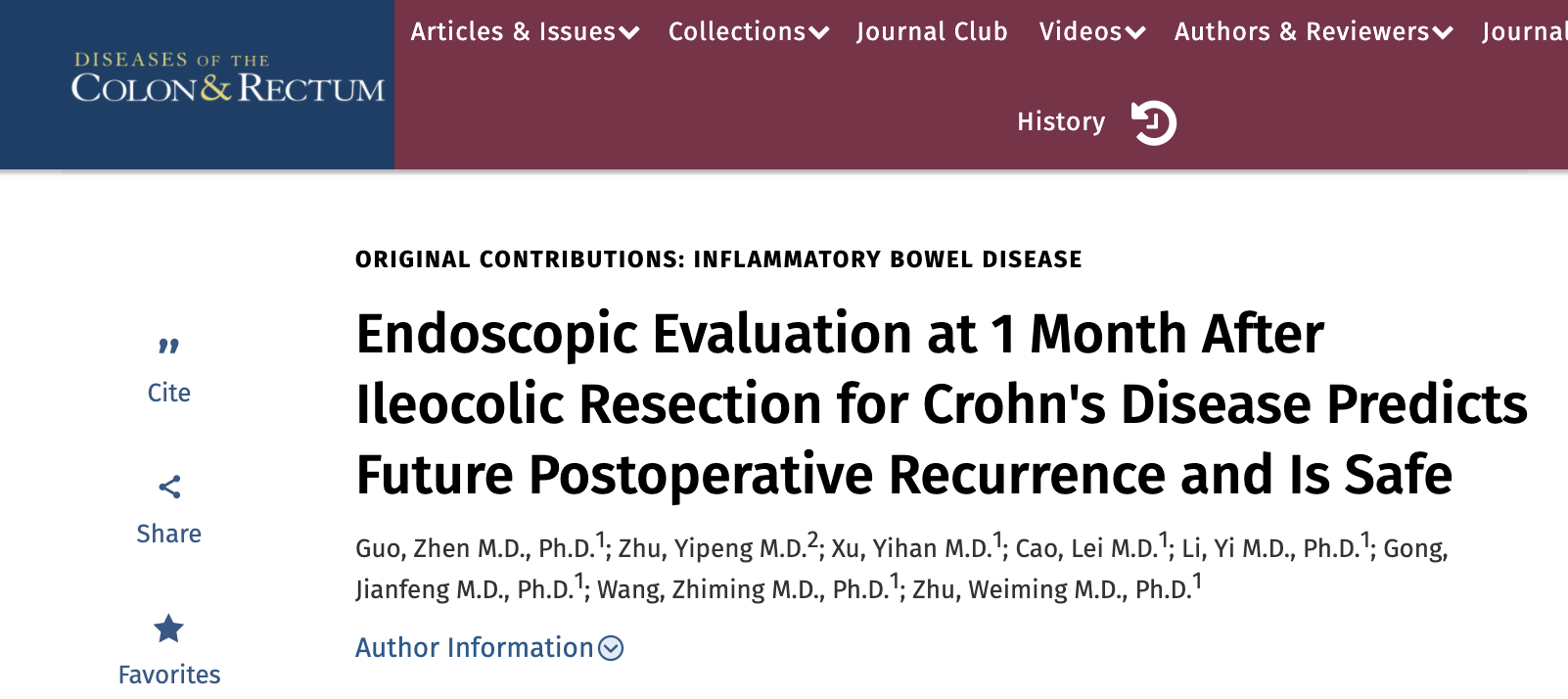
研究结果显示在总共84 次回结肠镜检查中,未发生内镜并发症。第一次评估的主要内镜检查结果为吻合口周围溃疡(10, 11.9%)、吻合口散在溃疡(35, 41.7%)、新末端回肠溃疡(16, 19.0%)、吻合口水肿(50, 59.5%) ,吻合口轻度狭窄 (7, 8.3%),新末端回肠轻度狭窄 (3, 3.6%)。吻合口散在溃疡与未来术后复发相关(OR,2.532(95% CI,1.02-6.32),p = 0.046)。术后第 14 天粪便钙卫蛋白 >150 ug/g 可预测吻合口散在溃疡 (OR, 2.91 (95% CI, 1.31–7.47), p= 0.027)。改良的 Rutgeerts 评分用于定义内镜检查结果:i0, 37 (44.0%); i1, 4 (4.8%); i2a, 29 (34.5%); i2b, 11 (13.1%); i3, 0; i4, 3 (3.6%)。评分≥i2a 与未来术后复发相关(OR,3.17(95% CI,1.22-8.27),p = 0.018)。在第一次内窥镜评估时,没有任何因素与 Rutgeerts 评分≥i2a 相关。
图:肠镜图片
本项研究结果证实在CD患者术后 1 个月内镜检查是安全的。近半数患者出现吻合口散在溃疡,并与未来术后复发有关。
原始出处:
Guo, Zhen. Et al. Endoscopic Evaluation at 1 Month After Ileocolic Resection for Crohn's Disease Predicts Future Postoperative Recurrence and Is Safe. Diseases of the Colon & Rectum.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#结肠切除术#
40
#切除术#
51
#术后复发#
46
#内镜#
42
✌🏽️
58