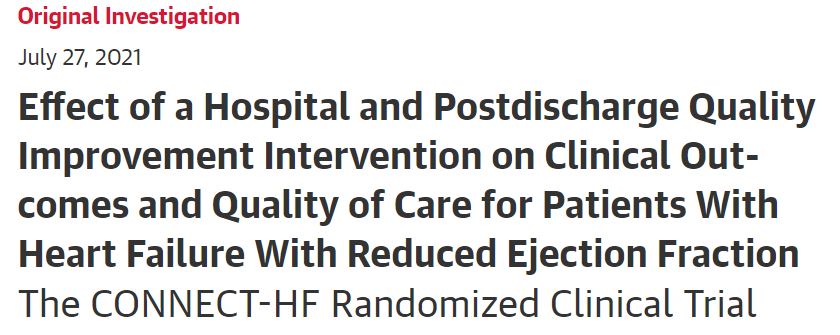
JAMA:住院前后护理质量干预措施对HFrEF心力衰竭患者临床结果的影响
2021-08-02 MedSci原创 MedSci原创
在随机接受医院和出院后质量改进干预与常规护理的HFrEF患者中,首次心衰再住院或死亡的时间或心衰护理质量综合评分的变化没有明显差异。
晚期心力衰竭(HF)是指HF患者即使接受了最大程度的循证治疗,仍持续出现影响日常生活的严重症状。晚期HF也称为“难治性”、“终末期”HF。患者的症状通常包括运动不耐受、非刻意的体重减轻、难治性容量超负荷、复发性室性心律失常,以及低血压和灌注不足的体征。
射血分数保留型心力衰竭(HFpEF)是指有HF的症状和体征,但左室射血分数(LVEF)正常或接近正常(LVEF≥50%)的临床综合征。大多数HFpEV患者的左室容积正常,有舒张期功能障碍的证据,例如左室充盈异常、充盈压升高。
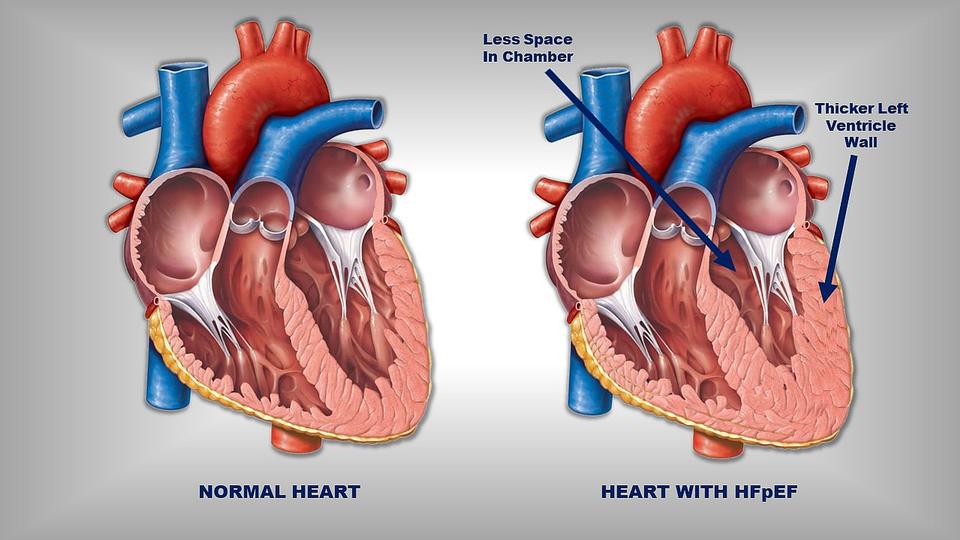
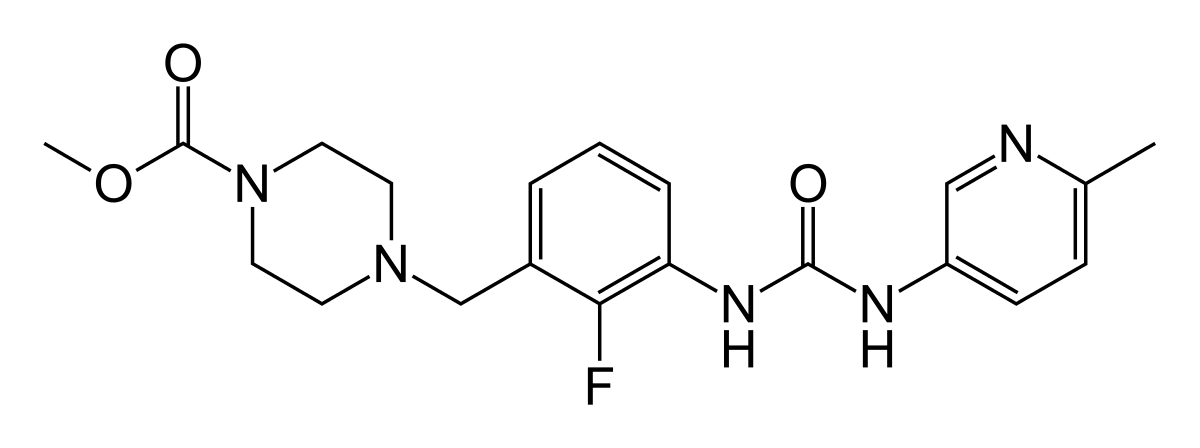
相比之下,射血分数降低型心力衰竭(HFrEF)的特点为左心室容积增加和射血分数降低。以前HFpEF称为“舒张性心力衰竭”,HFrEF称为“收缩性心力衰竭”。目前,关于HFpEF的临床试验迄今为止得到的结果是中性的,治疗主要针对相关疾病(如高血压)和症状(如水肿)。
HFpEF与HFrEF的治疗基于的证据不同,所以其管理方案也不同。临床试验结果表明,神经体液拮抗剂(如β受体阻滞剂、ACEI和ARB)和心脏再同步化治疗虽然对HFrEF有效,但不能减轻HFpEF的病况和死亡风险。这些资料表明,HFrEF与HFpEF的病理生理学基础有根本区别。
然而,改善指南指导下的药物治疗的干预措施未能持续达到目标指标,而且有限的数据可以为改善HF护理质量的努力提供参考。为此,来自杜克大学医学院的心血管专家评估了院内和出院后质量改进干预措施与常规护理相比对HF结果的影响,结果发表在JAMA杂志上。
这项分组随机临床试验在161家美国医院进行,包括5647名患者(2675名干预vs2972名常规护理),对HFrEF患者出院后进行跟踪。该试验从2017年至2020年进行,最终随访日期为2020年8月31日。
被随机分配到医院和出院后质量改进干预的医院(n = 82)接受由训练有素的HF和质量改进专家小组对临床医生的定期教育,以及对HF过程措施(例如,对HFrEF使用指南指导下的药物治疗)和结果的审计和反馈。主要结果是首次心衰再住院或全因死亡率的综合,以及基于机会的心衰质量综合评分的变化。
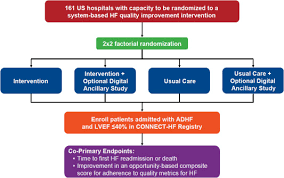
试验流程
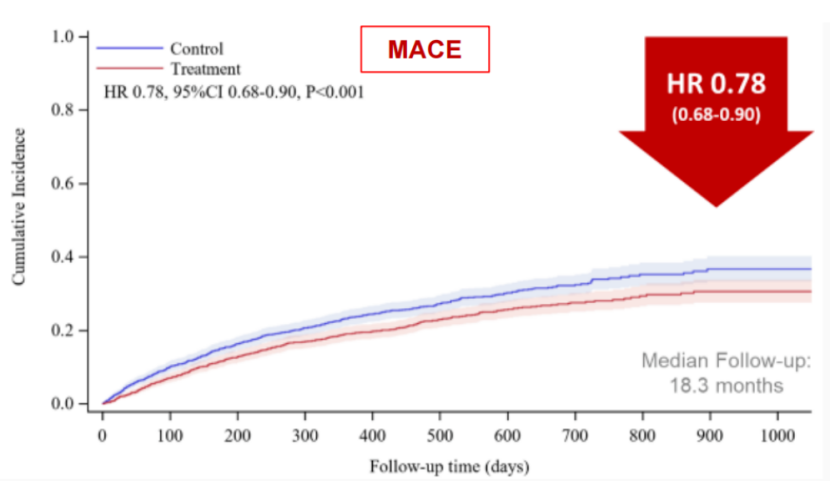
在5647名患者中(平均年龄63岁;33%为女性;38%为黑人;87%为慢性心衰;49%为近期心衰住院),5636人(99.8%)的生命状态是已知的。干预组有38.6%的人发生心力衰竭再住院或全因死亡,而常规护理组有39.2%,两组没有统计学差异(OR=0.92,95%CI:0.81-1.05)。
基线护理质量得分分别为42.1% vs 45.5%,从基线到随访的变化为2.3% vs -1.0%(差异=3.3% ,95% CI:-0.8%-7.3%),两组在最后一次随访时获得较高综合质量得分的几率没有明显差异(OR=1.06,95% CI, 0.93 - 1.21)。

出院随访期间发生主要结局事件的累积风险
综上,在随机接受医院和出院后质量改进干预与常规护理的HFrEF患者中,首次心衰再住院或死亡的时间或心衰护理质量综合评分的变化没有明显差异。
参考文献:
Effect of a Hospital and Postdischarge Quality Improvement Intervention on Clinical Outcomes and Quality of Care for Patients With Heart Failure With Reduced Ejection Fraction: The CONNECT-HF Randomized Clinical Trial. JAMA. 2021;326(4):314–323. doi:10.1001/jama.2021.8844
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#干预措施#
32
#院前#
35
#护理质量#
0
#临床结果#
34
#HFrEF#
46
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
40
受用了
67