European Radiology:进行性多发性硬化患者的脑血流量对全身动脉循环的依赖性
2022-08-24 shaosai MedSci原创
脑血管反应性(CVR)是一种调节机制,负责根据血管活性刺激和代谢需求的波动来重新分配脑血流。
多发性硬化症(MS)是一种中枢神经系统(CNS)的慢性神经退行性和炎症性疾病。在疾病的复发-缓解(RR)阶段经过一段时间后,损伤的积累和神经元的加速丧失导致了不可逆转的多发性硬化症进展期(PMS)。尽管多发性硬化症患者死亡时比较年轻,但与健康对照组相比,他们表现出更多的脑血管病变,包括更大的血管周围间隙扩张、动脉周围血色素沉着和髓鞘稀疏。
此外,与健康人相比,多发性硬化症患者的全身血管病变和脑小血管病变之间的联系要强得多。
脑血管反应性(CVR)是一种调节机制,负责根据血管活性刺激和代谢需求的波动来重新分配脑血流。越来越多的证据表明,这种神经血管单元的失效和解耦可以促进对更大灌注需求的反应受损,加剧线粒体压力、神经元病变和认知能力下降。
近日,发表在European Radiology杂志的一项研究测量并比较了临床孤立综合征(CIS)/RRMS和PMS患者的体内脑和全身动脉血流率,为临床进一步明确MS的疾病进展及病理生理提供了参考依据。
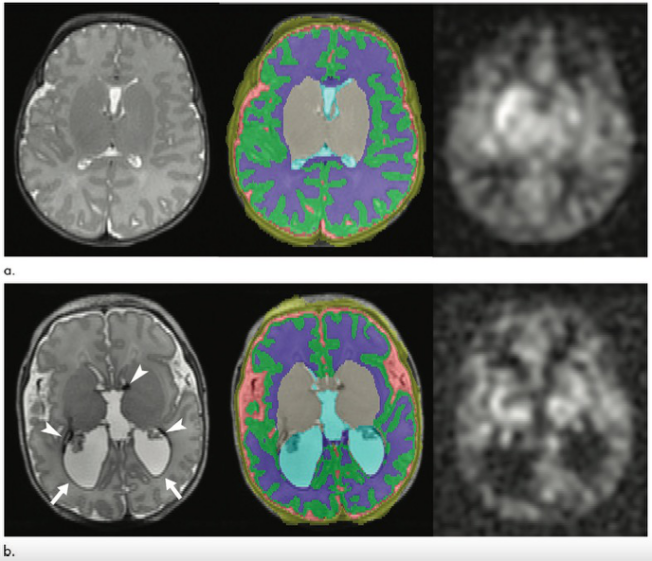
通过动态磁敏感对比灌注加权成像(DSC-PWI)和多普勒超声的MRI检查,分别对118名患者(75名临床孤立综合征(CIS)/复发性MS和43名进展性MS)进行了脑灌注和SABF评估。计算了正常外观的全脑(NAWB)和灰质(GM)的平均传输时间(MTT)和时间到峰值(TTP),单位为秒。通过双侧颈总动脉和椎动脉的血流(单位:毫升/分钟)代表SABF。全脑体积(WBV)和身体质量指数(BMI)被用作额外的协变量。
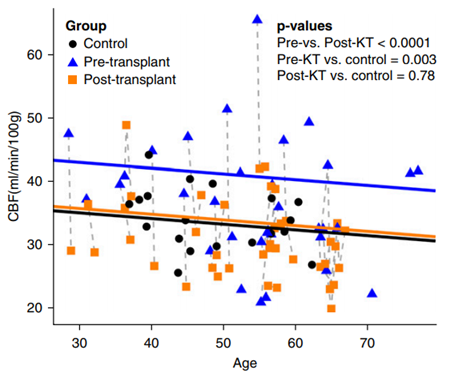
较高的收缩压与较低的SABF有关(-0.256,P = 0.006)。在全部MS样本中,较高的SABF与较短的NAWB(r = -0.256,p = 0.007和r = -0.307,p = 0.001)和GM(r = -0.239,p = 0.012和r = -0.3,p = 0.001)的MTT和TTP有关。SABF和TTP的关联是由PMS患者驱动的(r = -0.451, p = 0.004和r = -0.451, p = 0.011)。只有在PMS中,SABF仍然是NAWB(标准化β=-0.394,p=0.022)和GM TTP(标准化β=-0.351,p=0.037)的重要预测因素。与较高的四分位数相比,较低的SABF四分位数的患者的MTT和TTP明显较低(年龄、性别、BMI和WBV调整后的方差分析p < 0.025)。

图 基于SABF四分位数,PMS患者的上下肢表现的差异
本研究表明,代表PMS患者脑组织和GM血流总量与大脑的系统动脉输入有关。CIS/RRMS患者并没有显示出这种关系,表明PMS患者村早的CVR受损。无法补偿较低的SABF可能进一步推动MS临床预后的恶化。
原文出处:
Dejan Jakimovski,Niels Bergsland,Michael G Dwyer,et al.Cerebral blood flow dependency on systemic arterial circulation in progressive multiple sclerosis.DOI:10.1007/s00330-022-08731-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#脑血流#
51
#进行性#
42
#多发性#
38
#血流量#
35
#PE#
38