Nat Commun:利用细胞能量来进行癌症治疗
2014-03-19 Nature中文网 Nature中文网
能够利用一个癌细胞内的“能量分子”来触发药物在肿瘤所在位置的释放的一个药物载体,被发现能成功治疗小鼠的癌症。发表在本期Nature Communications上的这些发现也许能为治疗癌症提供另一个策略。Figure 1: Schematic design of the ATP-triggered Dox release system. 纳米颗粒能向肿瘤输送药物,但需要在选择性地定向肿瘤细胞方面
能够利用一个癌细胞内的“能量分子”来触发药物在肿瘤所在位置的释放的一个药物载体,被发现能成功治疗小鼠的癌症。发表在本期Nature Communications上的这些发现也许能为治疗癌症提供另一个策略。【原文下载】
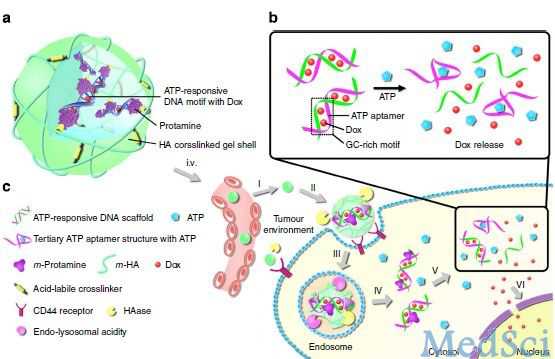
Figure 1: Schematic design of the ATP-triggered Dox release system.
纳米颗粒能向肿瘤输送药物,但需要在选择性地定向肿瘤细胞方面有所改进。癌细胞经常含有为代谢提供能量的高水平ATP,这一点有可能被用于治疗。Zhen Gu及同事描述了一种纳米颗粒载体,它利用高水平的ATP来触发化疗药物Doxorubicin的释放。在有ATP存在的情况下,该载体能发生形状变化,导致药物的释放。他们发现,在实验室中这种方法在培养的细胞内和在小鼠体内都能增强由Doxorubicin诱导的癌细胞死亡。这些发现可能会导致用于将化疗药物输送到癌细胞的新策略的问世。
原始出处:
Ran Mo,Tianyue Jiang,Rocco DiSanto,Wanyi Tai & Zhen Gu.ATP-triggered anticancer drug delivery.Nature Communications 5, Article number: 3364 doi:10.1038/ncomms4364 【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
40
#细胞能量#
38
#癌症治疗#
43
#COMMUN#
33