Nanoscale:上海交大六院汪泱教授利用水凝胶缓释干细胞外泌体促进关节软骨的再生
2017-03-15 外泌体之家 外泌体之家
关节软骨几乎没有先天自愈的再生能力是临床治疗中的巨大挑战。干细胞衍生的外泌体(SC-Exos)是一种重要类型的细胞外纳米泡,对于代替基于干细胞的治疗的软骨再生显示出巨大的潜力。目前还没有有效的给药方法能够在软骨缺损部位持久保留外泌体,有效发挥其修复作用;然而软骨再生通常需要相对长的时间。因此,在这项研究中,来自上海交通大学附属第六人民医院的汪泱研究员和华东理工大学的研究人员合作开发了光诱导亚胺交联
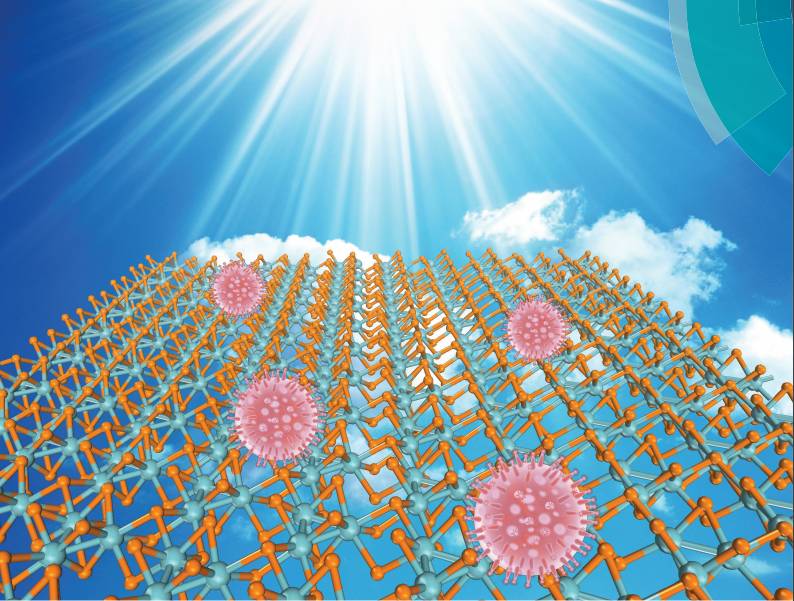
关节软骨几乎没有先天自愈的再生能力是临床治疗中的巨大挑战。干细胞衍生的外泌体(SC-Exos)是一种重要类型的细胞外纳米泡,对于代替基于干细胞的治疗的软骨再生显示出巨大的潜力。目前还没有有效的给药方法能够在软骨缺损部位持久保留外泌体,有效发挥其修复作用;然而软骨再生通常需要相对长的时间。因此,在这项研究中,来自上海交通大学附属第六人民医院的汪泱研究员和华东理工大学的研究人员合作开发了光诱导亚胺交联水凝胶胶,呈现出优良的操作能力、生物相容性和最重要的软骨整合能力,可作为外泌体支架用作软骨再生的无细胞组织补丁(EHG)。研究发现EHG可以将SC-Exos保留在内部并在体外正调节软骨细胞和hBMSCs。此外,EHG可以与自身软骨基质整合,并促进细胞沉积在软骨缺损部位,最终促进软骨缺损修复。希望EHG组织补丁将提供一种新的无细胞支架材料用于帮助伤口修复。
参考文献:
Liu X, Yang Y, Li Y, et al. Integration of Stem Cell-Derived Exosomes with In Situ Hydrogel Glue as a Promising Tissue Patch for Articular Cartilage Regeneration[J]. Nanoscale, 2017. IF=7.76
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#scale#
36
#关节软骨#
41
#水凝胶#
39
#凝胶#
26
#上海交大#
35
研究创新性很强
68