Psychooncology:年轻乳腺癌患者的性生活质量下降
2015-02-28 Jessie 译 MedSci原创
v\:* {behavior:url(#default#VML);} o\:* {behavior:url(#default#VML);} w\:* {behavior:url(#default#VML);} .shape {behavior:url(#default#VML);} Normal
乳腺癌患者中绝经前的患者高达1/4,随着医疗技术的发展,这些患者治疗后生存期逐渐延长,生活质量成为关注的焦点。其中性生活对于年龄的患者而言尤其重要。韩国首尔大学的研究者调查了在乳腺癌诊断前性行为活跃的年轻乳腺癌存活者的性行为和性功能的改变,并探讨了对性行为产生不良影响的危险因素。研究结果发表于近期的PSYCHO-ONCOL杂志上。
研究对象为尚未绝经且患乳腺癌之前性行为活跃的早期乳腺癌患者,共304名。通过问卷调查来评估患者的性行为和性功能,性行为是通过自设的问题询问患者过去6个月中是否有至少每月一次的规律的性生活,如果回答否就认为该患者性行为不活跃;性功能所用的问卷是女性性功能指数(Female Sexual Function Index), 该指数小于3说明存在性功能方面的问题。在手术后通过回顾的方式评估患者在患乳腺癌之前的性行为和性功能情况,第二次调查时间是完成化疗或激素治疗后至少12个月。
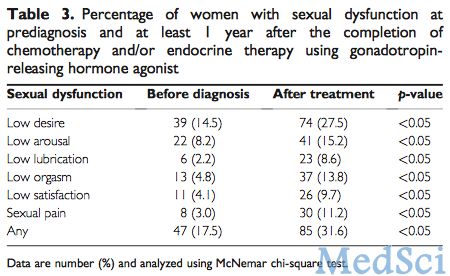
患者的中位年龄为46岁,范围为23~57岁。其中35人(11.5%)治疗后出现性行为不活跃,在剩下的269名性行为仍保持活跃的患者中,31.6%的患者存在性功能障碍,包括低性欲(27.5%),低性唤起(15.2%),低性高潮(13.8%),低满意度(9.7%)等。治疗后出现性功能障碍的患者比例显著高于患病前的患者比例(31.6% vs. 17.5%,P<0.05)。多元Logistic回归分析显示,化疗引起的绝经(OR=4.28,95%CI:1.37~13.34)、甲状腺功能紊乱(OR=3.82,95%CI:1.05~13.90)及抑郁(OR=2.87,95%CI:1.07~7.72)是性行为不活跃的独立危险因素。化疗引起的绝经是性功能障碍的主要危险因素(OR=2.81~5.46,P<0.05)。
结论:化疗引起的绝经与治疗后乳腺癌患者的性行为不活跃及性功能障碍均有关。甲状腺功能紊乱和抑郁是年轻乳腺癌患者性行为不活跃的危险因素。
原始出处
Lee M, Kim YH, Jeon MJ. Risk factors for
negative impacts on sexual activity and function in younger breast cancer
survivors. Psychooncology. 2015 Feb 17. doi: 10.1002/pon.3772. [Epub ahead of
print]
本文是MedSci编译,欢迎授权后转载,非常感谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











已拜读,受益匪浅。
50
#年轻乳腺癌#
49
好棒
119
很不错学习了
120
#Oncology#
27
#Oncol#
26
#乳腺癌患者#
21
#性生活#
26
题目不错
120