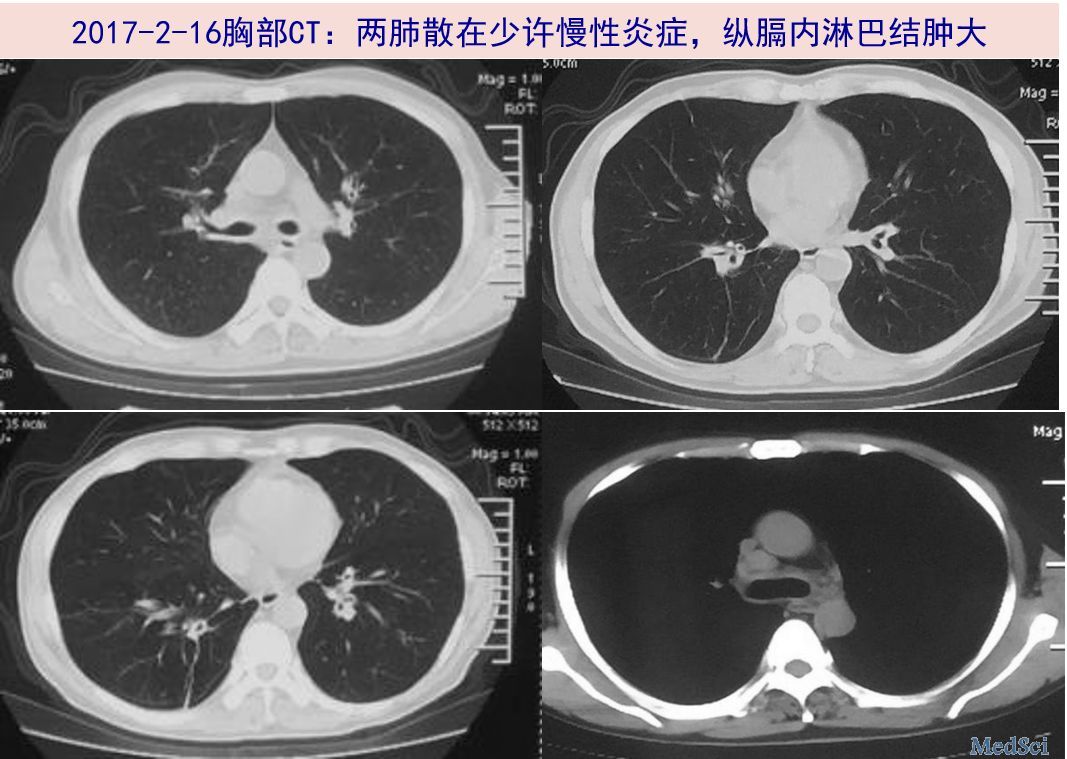
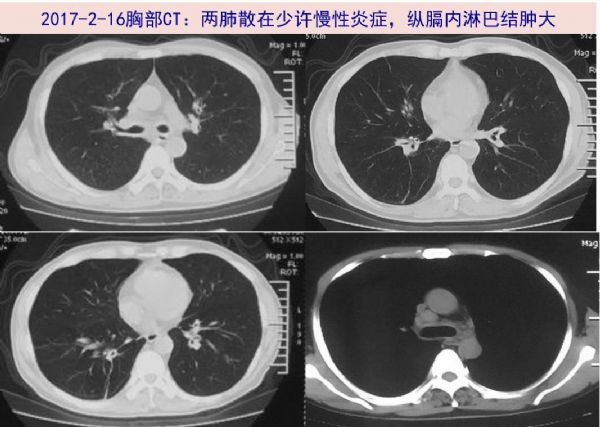
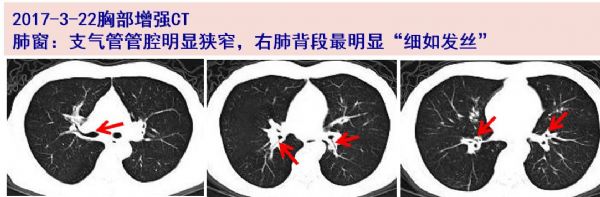
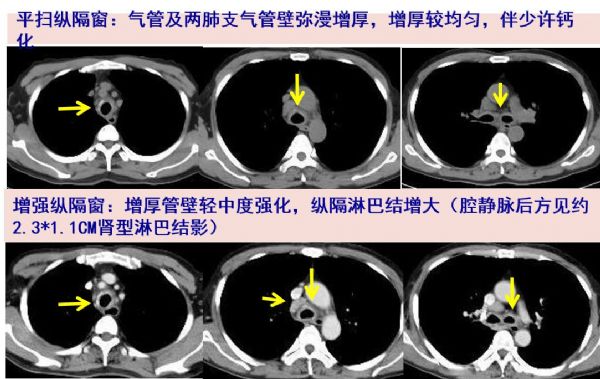
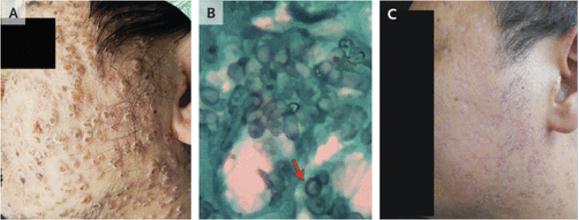
病例分享:咳嗽2月抗生素治不好,精检查细分析发现罕见妖孽!
2018-02-05 马玉燕、金文婷 SIFIC感染官微
2017年1月初着凉后出现咳嗽伴少量白粘痰,无发热、气促等不适。因原有哮喘史,故予舒利迭、普米克都保治疗,但无缓解,遂于1月中旬至当地医院予左氧氟沙星0.5g qd+甲强龙 40mg qd静滴,4天后症状好转。停药3天后再次出现咳嗽咳痰,予莫西沙星0.4g qd+ 甲强龙 40mg qd静滴,5天后好转。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











谢谢分享
60
#罕见#
33
学习谢谢分享
62
了解了解.继续关注
69
感染
59
学习了
55
学习了
26
谢谢分享.学习受益匪浅
26
很好的学习材料.对临床和科研都有很大帮助作用.水滴石穿.不断积累.
0
很好的学习材料.对临床和科研都有很大帮助作用.水滴石穿.不断积累.
24