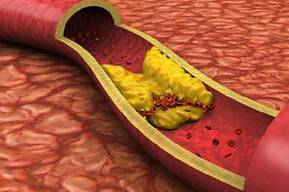
Atherosclerosis: baPWV与缺血性卒中患者的预后相关
2016-11-05 MedSci MedSci原创
背景:臂踝脉搏波传导速度(baPWV)是测量动脉僵硬度的良好指标,且与未来发生心血管事件的风险相关。本研究旨在探讨baPWV是否可以预测卒中后3个月的功能预后。方法:这项基于医院的研究包括327例缺血性卒中患者,住院期间测量baPWV。其中,良好和较差的功能预后为卒中后3个月内,改良Rankin评分<3和≥3。结果:预后不良的患者与高龄,(73.1 vs 66.3岁,P<0.001),更可能有颈动
背景:臂踝脉搏波传导速度(baPWV)是测量动脉僵硬度的良好指标,且与未来发生心血管事件的风险相关。本研究旨在探讨baPWV是否可以预测卒中后3个月的功能预后。
方法:这项基于医院的研究包括327例缺血性卒中患者,住院期间测量baPWV。其中,良好和较差的功能预后为卒中后3个月内,改良Rankin评分<3和≥3。
结果:预后不良的患者与高龄,(73.1 vs 66.3岁,P<0.001),更可能有颈动脉狭窄(29.5% vs 13.1%,P<0.001),房颤(21% vs 11.3%,P = 0.020),冠状动脉疾病史(20% vs 11.7%,P = 0.042),和高baPWV值(22.84 vs 19.48 m/s,P<0.001)。不论患者的年龄、性别、基线危险因素,卒中的严重程度,以及脑卒中病因,预后不良的患者中,baPWV较高。多因素分析显示ROC计算,baPWV > 23.11m/Ss 是功能预后不良的独立预测价值(OR,1.51;95%CI,1.08-2.11;P = 0.016)。
结论:在脑卒中急性期测量baPWV可独立预测3个月的功能预后。研究表明,baPWV可作为早期识别严重卒中相关残疾的患者。
原始出处:
Ishizuka K, Hoshino T,et al. Brachial-ankle pulse wave velocity is associated with 3-month functional prognosis after ischemic stroke. Atherosclerosis. 2016 Aug 26
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#缺血性卒中患者#
37
#缺血性卒#
32
#Sclerosis#
29
#卒中患者#
33
#缺血性#
28
#ROS#
34