ESC 2015:左心耳电隔离可抑制长程持续性房颤(BELIEF研究)
2015-09-01 MedSci MedSci原创
ESC2015年会“Hot Line”专题会上公布的BELIEF研究结果显示,对于经过标准治疗但仍有长程持续性房颤的患者,给予额外的左心耳电隔离可减少房颤发生而且不增加并发症。Luigi Di Biase博士(美国德克萨斯St. David's医学中心心律失常研究所)等报告,与标准消融治疗相比,在此基础上加左心耳电隔离可以提高导管消融的远期成功率。BELIEF研究纳入173名长程持续性房颤患者。长
ESC2015年会“Hot Line”专题会上公布的BELIEF研究结果显示,对于经过标准治疗但仍有长程持续性房颤的患者,给予额外的左心耳电隔离可减少房颤发生而且不增加并发症。Luigi Di Biase博士(美国德克萨斯St. David's医学中心心律失常研究所)等报告,与标准消融治疗相比,在此基础上加左心耳电隔离可以提高导管消融的远期成功率。
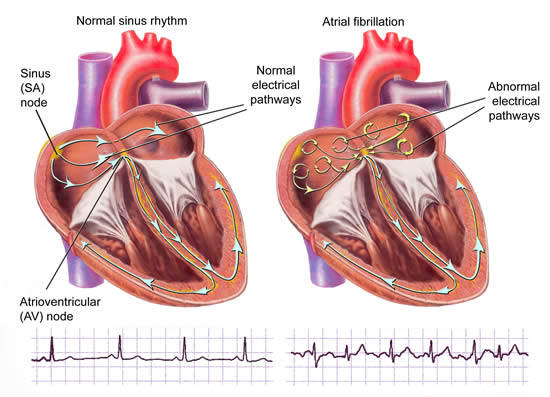
BELIEF研究纳入173名长程持续性房颤患者。长程持续性房颤定义为房颤持续时间大于12个月。患者被随机分配到两组:标准消融治疗组(肺静脉电隔离[PVI]+消融额外的肺动脉触发点,n=88)和标准消融治疗+左心耳电隔离组(n=85)。主要终点为1年时房颤复发。
结果显示,标准消融治疗组1年时28%的患者无复发,标准消融治疗+左心耳电隔离组为56%(HR 1.92; p=0.001)。对于两组中复发的患者给予左心耳电隔离。24个月时,经过平均1.3次治疗,两组累积成功率分别为56%和76%(HR 2.24; p= 0.003)。
两组患者并发症(包括TIA/卒中)发生率无差异。标准消融治疗+左心耳电隔离组平均射频时间延长(93 vs 77 minutes; P<0.001)。
多因素分析显示,无左心耳电隔离与房颤复发率显著升高相关(HR 2.2; p = 0.004)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#持续性#
39
#BELIEF研究#
46
#电隔离#
38
感谢作者分享
92
學習
122
#左心耳#
29