72岁,女性,既往无特殊。
因为急性缺血性卒中入院。
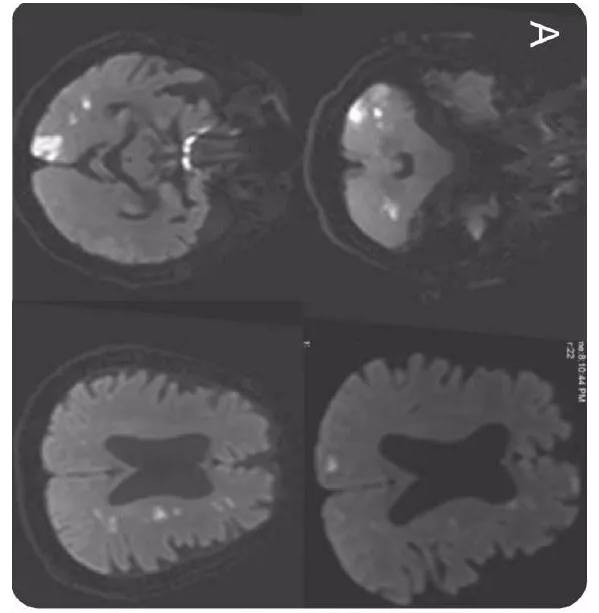
头MRI DWI可见前后循环多支动脉分布区梗死。因为血沉(98 mm/h)快,随后进行了颞浅动脉超声和DSA检查。
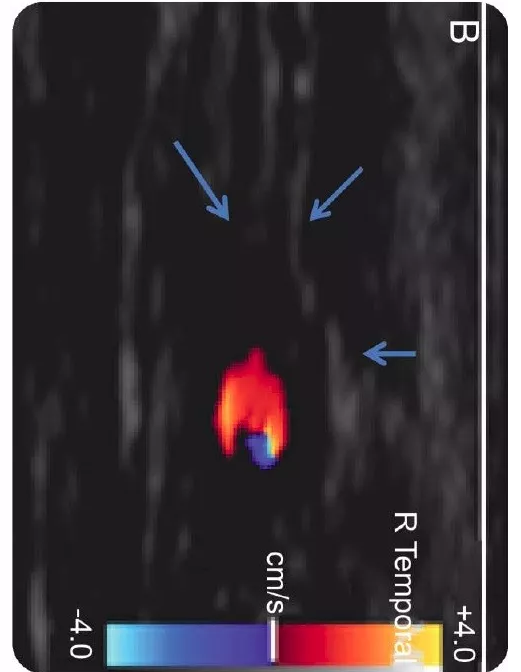
下图A,DWI显示多发梗死;下图B多普勒超声显示右侧颞浅动脉低回声月晕征(hypoechoic halo)(箭头为动脉壁):
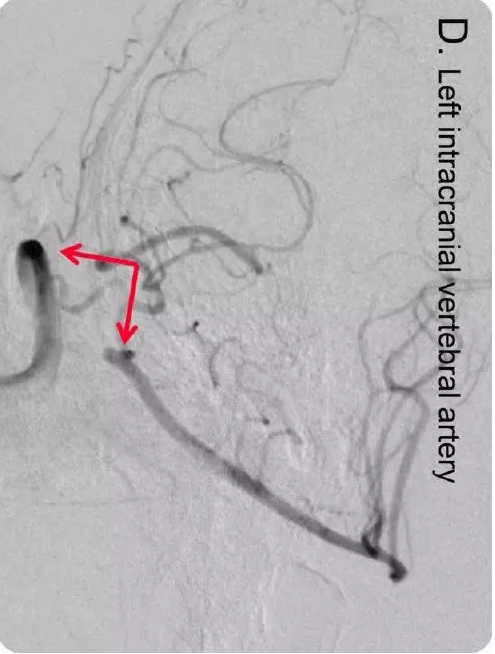
下图为DSA,显示颈内动脉颅内段(图A和B)和椎动脉(图C和D)严重狭窄。右侧颞浅动脉也受累(图A,三角箭头),左侧颞浅动脉未受累(图B,三角箭头):



颞浅动脉活检显示CD3+/炎症细胞和弹力层破碎(图C和D):

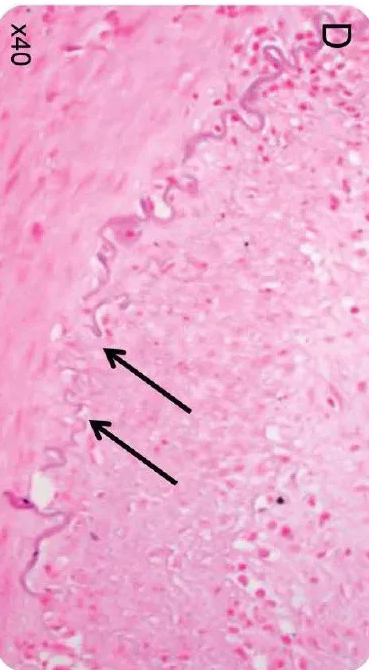
最终活检诊断为巨细胞动脉炎。
原始出处:
Odysseas Kargiotis,et al. Teaching NeuroImages: Giant cell arteritis presenting with acute ischemic strokes due to diffuse intracranial stenoses. Neurology. 2017 Oct 10
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#Neurol#
36
#动脉炎#
36
#巨细胞#
38