Cell Death Differ+Cardiovasc Res:发现血小板寿命与功能调控新机制
2019-02-13 MedSci 北京大学
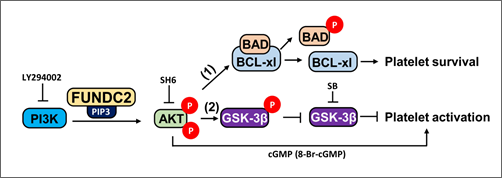
近日,北京大学分子医学研究所马淇博士与合作者分别在Cell Death and Differentation(CDD)和Cardiovascular Research(CVR)上发表最新研究成果,鉴定了一个调控血小板寿命和功能的新分子,并研究了其调控机制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
25
#CEL#
36
#ASC#
26
#Differ#
36
#Death#
21