Cancers:我们对0 - 10岁尤文肉瘤骨骼发育不全儿童的生存率了解多少?
2022-04-09 从医路漫漫 MedSci原创
尤文肉瘤预后较差的已知风险因素是位于骨盆或脊柱和胸壁的原发性肿瘤,以及较大的肿瘤体积(> 200 mL)和大小(> 8cm)和转移性疾病的存在。
背景:尤文肉瘤(ES)是一种侵袭性骨和软组织肿瘤,主要影响儿童和年轻人。15-20%的患者在诊断时年龄在0-10岁之间。尤文肉瘤多模式治疗的进展已经逐渐将无转移的尤文肉瘤的生存率提高到70-75%的10年总生存率。转移性尤文肉瘤的存活率仍然很低,5年OS为20-35%
尤文肉瘤预后较差的已知风险因素是位于骨盆或脊柱和胸壁的原发性肿瘤,以及较大的肿瘤体积(> 200 mL)和大小(> 8cm)和转移性疾病的存在。肺外转移的患者明显比单纯肺转移的患者更差。相反,在多变量分析中,年龄越小,临床结果越好,尤其是10岁以下。
尚不清楚为什么10岁以下的尤文肉瘤患儿会有更好的存活率。一项大型研究表明,幼儿(0至9岁)不太可能出现骨盆或脊柱的原发性肿瘤,在诊断时也不太可能出现转移性疾病。然而,年龄是否具有独立于其他预测预后不良的变量(如转移性疾病和肿瘤部位)的预后价值仍不清楚。然而,10岁以下患者的良好存活率强调了最小化长期发病率和调查治疗负担的需要。个体化胚胎干细胞治疗应根据总体估计存活率、经历的治疗负担和预测的晚期后遗症来决定。
方法:在这项回顾性多中心研究中,纳入了1982年至2008年间在荷兰的四个肉瘤中心(n = 33)和西班牙的一个肉瘤中心(n = 27)接受治疗的所有0-10岁的连续ES患者,随访时间至少为10年。计算OS、无局部复发生存率(LRFS)和无远处转移生存率(DMFS)。分析影响OS的潜在因素(危险因素和保护因素)。
结果:60例患者中位随访时间为13.03年。所有患者均接受化疗联合局部治疗,其中30例(50%)患者接受单纯手术,12例(20%)患者接受单纯放疗,或18例(30%)患者接受手术加放疗(12例术前,6例术后)。93%的患者实现了保肢。10-OS,-LRFS和-DMFS分别为81% (95%可信区间:71–91%)、89% (95%可信区间:85–93%)和81% (95%可信区间:71–91%)。6例患者出现LR,其中2例随后出现DM;所有患者都患有中轴ES(骨盆、脊柱或胸壁),这些患者都已死亡。10名患者发展为糖尿病;8例死于进行性疾病,2例目前处于缓解期,均仅伴有肺转移。阴性或广泛切除切缘与较好的OS显著相关。年龄< 6岁,肿瘤体积< 200 mL,无转移性疾病,2000年后的治疗显示出较好的OS趋势。两名患者出现继发性恶性肿瘤;两人都接受了化疗和确定性放疗的局部治疗。
表1 每个治疗组中死亡患者的数量。

表2 诊断时1和手术时2的单变量Cox回归分析结果。
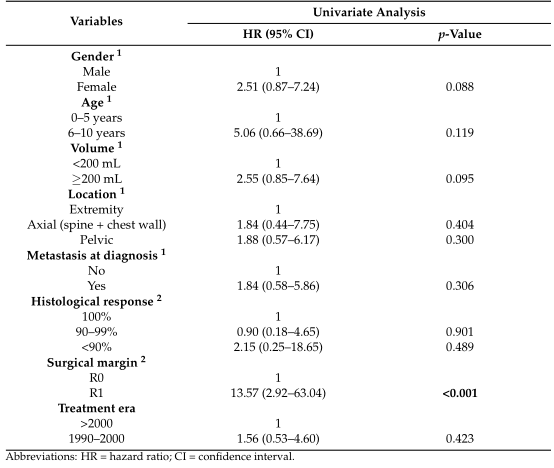

图1 年龄(A)、肿瘤体积(B)、诊断时的转移(C)、肿瘤位置(D)、手术切缘(E)和治疗时间(F)的Kaplan-Meier曲线
结论:这些最年轻的ES患者的总体存活率非常好。超过90%的患者进行了保肢手术。广泛的切除边缘是与较好的存活率显著相关的唯一因素。
原文出处:Bosma SE, van der Heijden L, Sierrasesúmaga L,et al.What Do We Know about Survival in Skeletally Premature Children Aged 0 to 10 Years with Ewing Sarcoma? A Multicenter 10-Year Follow-Up Study in 60 Patients.Cancers (Basel) 2022 Mar 12;14(6)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ERS#
40
#生存率#
40
#发育#
32
#尤文肉瘤#
52