Stroke:血管内血栓切除术后的血压变化轨迹与患者结局
2021-11-16 MedSci原创 MedSci原创
急性缺血性卒中患者在EVT后的前72小时内表现出不同的SBP变化轨迹,这些轨迹与功能结局有不同的关联。
血管内血栓切除术(EVT)后血压升高与出血性转化风险增加和功能预后不良相关。然而,EVT后的最佳血流动力学管理仍然未知,缺血性卒中急性期的血压管理过程尚未得到很好的归纳。

近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,该研究旨在明确EVT后具有不同血压变化轨迹的患者亚组,并研究它们与影像学结果和功能结局之间的关联。
这项多中心回顾性队列研究纳入了连续就诊的接受EVT的前循环大血管闭塞性缺血性卒中患者。在取栓后的前72小时内重复记录血压数据。潜在变量混合模型将受试者分为具有不同手术后收缩压(SBP)轨迹的五组。该研究的主要结局是功能状态,在卒中后90天使用改良的Rankin量表进行测量。次要结局包括出血性转化、有症状的颅内出血和死亡。
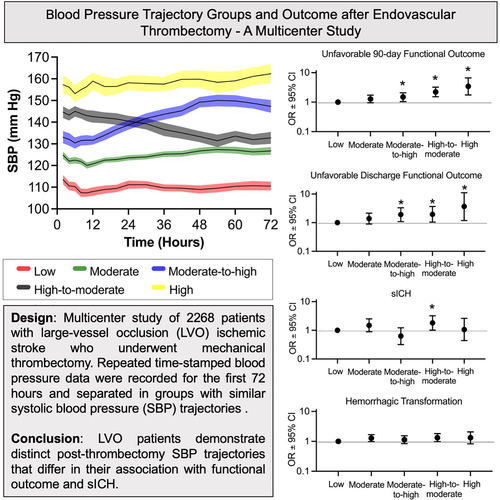
该研究有2268名患者(平均年龄[±SD]为69±15,美国国立卫生研究院卒中量表评分平均为15±7)被纳入分析。观察到五个不同的SBP变化轨迹:低(18%)、中(37%)、中到高(20%)、高到中(18%)和高(6%)。在调整潜在混杂因素后,SBP变化轨迹与90天时的功能结局独立相关(P<0.0001)。具有高和中高SBP变化轨迹的患者出现不良结局的几率显著更高(调整后的比值比为3.5[95%CI为1.8-6.7],P=0.0003,调整后的比值比为2.2[95%CI为1.5]–3.2],分别为P<0.0001)。高至中度组的受试者出现症状性颅内出血的风险增加(调整后的比值比为1.82[95%CI为1-3.2];P=0.04)。轨迹组与出血性转化之间未发现显著的关联。
由此可见,急性缺血性卒中患者在EVT后的前72小时内表现出不同的SBP变化轨迹,这些轨迹与功能结局有不同的关联。这些结果可能有助于确定未来血压调节试验的潜在候选人。
原始出处:
Nils H. Petersen.et al.Blood Pressure Trajectory Groups and Outcome After Endovascular Thrombectomy: A Multicenter Study.stroke.2021.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.034408
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#切除术#
39
#变化轨迹#
36
#血压变化#
49
#血栓切除#
42
#血栓切除术#
51
#患者结局#
34
#血管内血栓切除术#
39