联合国发布最新艾滋病报告
非洲年轻女性尤易感染

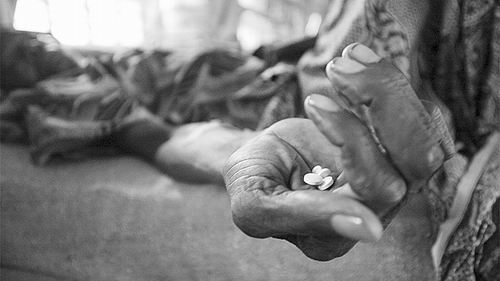
有1820万人正在接受ARV治疗。
图片来源:ton koene/Alamy Stock Photo
本报讯 根据瑞士日内瓦联合国艾滋病规划署(UNAIDS)的年度世界艾滋病日报告,当涉及到艾滋病病毒(HIV)的感染时,生活在撒哈拉以南非洲地区的年轻妇女正在经历着一个“特别危险的时间”。该报告同时指出,截至2016年6月,全球约1820万HIV感染者接受了抗逆转录病毒药物(ARV)治疗,获得这一“救命疗法”的患者人数较2010年约翻了一番。
这份报告指出,在2015年全世界范围内210万新增艾滋病病例中,大约有19%的患者是年龄在15岁至24岁的女性。该群体去年全球每周新增约7500名感染者。并且与同年龄的男性相比,在某些地区,年轻女性染病的风险更高。例如,在非洲南部,91%的新发感染病例为15岁至19岁的年轻女性。UNAIDS执行董事Michel Sidibé表示:“这一年龄段的年轻女性最不容易进行HIV测试,并且也很难了解她们的状态。这真的很不可思议。”
根据这份报告,造成这一结果的原因非常复杂。许多年轻女性并没有察觉到自己处于危险之中,并且她们生活在被UNAIDS称为“具有挑战性的环境”中,无法获得足够的食物和教育。并且,她们当中的很多人都与年长的男性发生过性关系。
与过去几年相比,更新后的世界艾滋病日(12月1日)对这种传染病提供了更加细致入微的观察。这份报告第一次考察了艾滋病在4个年龄段的发病情况,这被称为“对于HIV的生命周期方法”。UNAIDS建议这一分类——0岁到14岁、15岁到24岁、25岁到49岁以及50岁以后——能够带来针对这种传染病的“复杂动力学”更为清晰的了解,以及更具指向性的反应。该报告同时包括注射毒品者、男性同性恋、性工作者和变性人等在内的高危人群感染HIV的风险和接受治疗的最新情况。
其中最令人惊讶的细节之一是在2015年新增的15万儿童艾滋病病毒感染者中(其中半数儿童通过母乳喂养途径感染病毒),仅尼日利亚就占了1/4。Sidibé表示,对于这一发现,他的“失望比惊讶更多”。他说:“这是包括我个人在内的集体的失败。”
在南非,超过95%的感染HIV的孕妇接受了挽救生命的ARV治疗,这同时也能够预防母婴传播(MTCT)。尼日利亚正在分析它的数据,但UNAIDS表示,最新的数据意味着该国约有30%感染HIV的孕妇接受了ARV治疗。
根据这份报告,其他趋势则令人感到鼓舞。据估计,全世界3670万HIV感染者中,有一半(1820万人)接受了ARV治疗。在2010年至2015年之间,全球儿童新发艾滋病人数下降了51%,这要归功于广泛开展的防止MTCT项目。年度艾滋病相关死亡人数从2010年的200万下降至110万。
报告说,ARV可帮助HIV感染者活得更长久。在发展中国家与发达国家,艾滋病患者的寿命都得到了普遍延长,而这要感谢有效的ARV治疗。其中艾滋病感染者中最年长的组别——50岁以上的人数在增长,如今占全部感染人数的17%。如果艾滋病治疗能够像预期的那样变得更为普及,在未来4年中,艾滋病感染者的数量在这个最老的年龄段可能增加到47%。
此外报告指出,2014年全球约45%的新增感染者为“关键人群”及其性伙伴。报告警示,注射毒品者、男性同性恋及其他有男男性行为的人群中新增感染者数量继续上升,性工作者和变性人中新增感染者数量也未能实现下降。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












希望疫苗早日生产
58
#联合国#
49
很好的知识
46
应该做一个更好的研究。
58
谢谢分享,学习了
49
很好,不错,以后会多学习
49