EUR J CANCER:多西紫杉醇 vs多西紫杉醇联合卡铂治疗去势难治性前列腺癌的随机II期临床试验:RECARDO试验
2017-12-20 MedSci MedSci原创
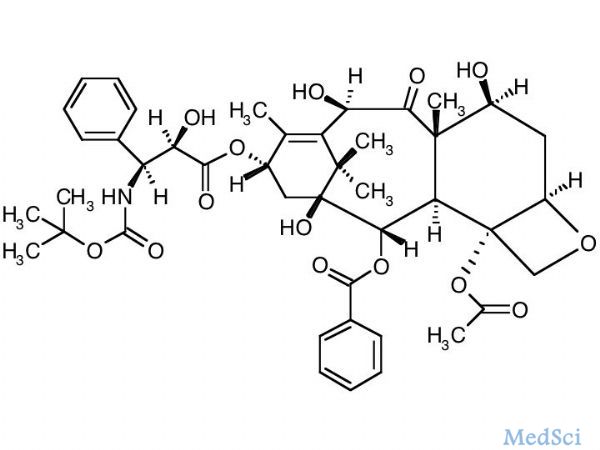
多西紫杉醇(Docetaxel)作为一种转移性去势难治性前列腺癌(mCRPC)的一线治疗药物,目前还没有一项前瞻性随机对照试验对其进行详细研究。近日荷兰学者便进行了一项这样的临床试验,他们对既往接受过多西紫杉醇治疗的前列腺癌患者继续使用多西紫杉醇及多西紫杉醇联合卡铂治疗。
多西紫杉醇(Docetaxel)作为一种转移性去势难治性前列腺癌(mCRPC)的一线治疗药物,目前还没有一项前瞻性随机对照试验对其进行详细研究。近日荷兰学者便进行了一项这样的临床试验,他们对既往接受过多西紫杉醇治疗的前列腺癌患者继续使用多西紫杉醇及多西紫杉醇联合卡铂治疗。
研究者们将先前经多西紫杉醇治疗后无瘤期>3个月的患者随机分为西紫杉醇组(75 mg/m2)和西紫杉醇(60 mg/m2)联合卡铂组。由于入组患者数不足预期(招募患者75名,而预期招募150名),该项临床试验提前终止,对于已经得到的结果,研究者们对比了无恶化生存期(PFS)和总生存率(OS)这两项数据,结果显示,对于多西紫杉醇单药治疗组,PFS中位数为12.7个月,对于多西紫杉醇联合卡铂组,PFS中位数为11.7个月;对于多西紫杉醇单药治疗组,OS中位数为18.5个月,对于多西紫杉醇联合卡铂组,OS中位数为18.9个月。统计数据显示,单药治疗和联合治疗并无显著差异,且感染及胃肠道不良反应发生率在联合治疗组中更高,研究者分析称,联合治疗可能导致了患者体内正常细胞受到攻击,因此多西紫杉醇单药治疗经证明更为有效,安全。
原始出处:
Esther W, H. Pieter et al. “A randomised phase
II trial of docetaxel versus docetaxel plus carboplatin in patients with
castration-resistant prostate cancer who have progressed after response to prior
docetaxel chemotherapy: The RECARDO trial”. European Journal of Cancer 2018. doi.org/10.1016/j.ejca
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#I期临床试验#
36
#铂#
29
#II期临床试验#
36
#I期临床#
29
#卡铂#
49
#II期临床#
37
#难治性#
33
#多西紫杉醇#
26