2019 ESMO 瑞戈非尼120 mg联合紫杉醇二线治疗晚期食管胃癌,初显疗效
2019-10-03 佚名 肿瘤资讯
2019年欧洲肿瘤内科学会(ESMO)年会在西班牙巴塞罗那隆重举行。靶向联合治疗作为当前的肿瘤治疗趋势,有多项研究在会上发布。其中一项Ⅰb期的REPEAT研究(798P)探索了瑞戈非尼联合紫杉醇用于晚期食管胃癌二线或以上治疗,显示出良好的安全性和有前景的疗效。
798P - Regorafenib in combination with Paclitaxel for beyond first-line treatment of advanced esophagogastric cancer (REPEAT): a phase Ib trial with expansion cohort
背景
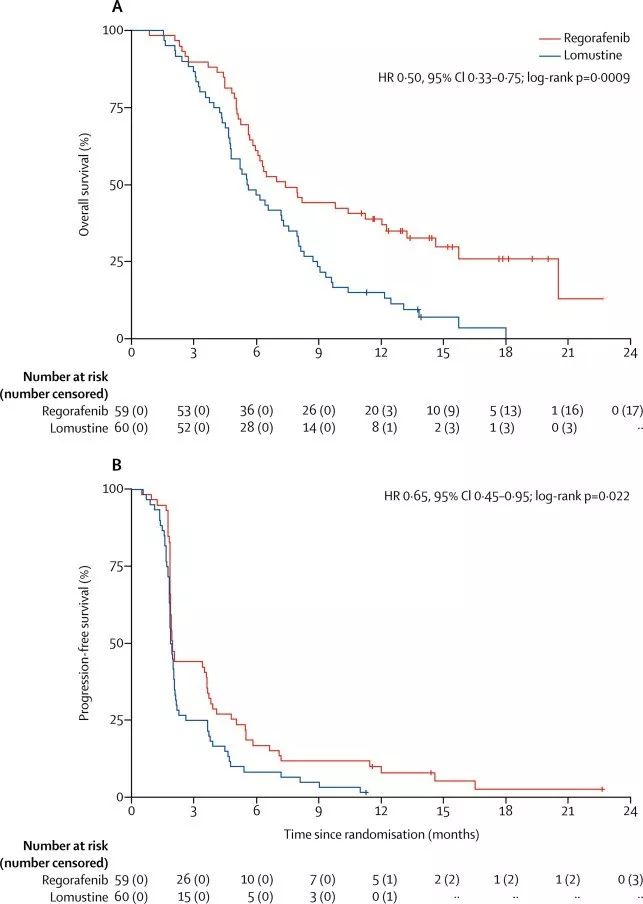
晚期食管胃癌(EGC)预后差,生存期不超过1年。诸如抗血管生成药物雷莫芦单抗联合紫杉醇这样的二线治疗使患者预后得到了改善。瑞戈非尼是一个靶向血管生成、肿瘤间质和激酶的多靶点激酶抑制剂,单药用于晚期胃癌可以改善患者的无进展生存(PFS)。这项REPEAT 研究评估了瑞戈非尼联合紫杉醇用于晚期EGC患者二线或以上治疗的最大耐受剂量和安全性。
方法
研究入组了一线治疗进展后的晚期食管癌、胃食管结合部癌或胃癌。要求患者既往接受过≥1线治疗(包括5-FU和含铂方案),ECOG PS 0~1分。研究分为剂量爬坡队列和剂量扩展队列。剂量爬坡队列采用3+3模式,瑞戈非尼剂量分别为80 mg/d、120 mg/d和160 mg/d;剂量扩展队列中,采用瑞戈非尼120 mg/d,d1~21天用药,联合紫杉醇 80 mg/m2,d1、d8和d15,28天为一个治疗周期。采用RECIST 1.1标准,每2周进行一次疗效评价;在治疗的每个周期均评估剂量限制性毒性(DLT),毒性评估采用CTCAE v4标准。扩展队列中,分别在第1周期第1和15天采集药代动力学标本;第1和15天在注射紫杉醇后进行转移灶活检。
结果
在瑞戈非尼80 mg/d剂量组中(n=3),未观察到DLT;在120 mg/d剂量组中(n=7),观察到1例患者出现3级手足综征;在160 mg/d剂量组中(n=4),3级腹泻、3级口腔炎和3级GGT升高的患者分别为1例、2例和1例。因此,确定瑞戈非尼最大耐受剂量为120 mg/d。
2015至2018年,研究从3个中心入组了48例患者,其中剂量爬坡队列和剂量扩展队列分别为14例和34例。入组患者的中位年龄为64岁,男性占81%,食管癌、胃癌和胃食管结合部癌分别占44%、19%和38%。大多数患者(60%)在二线接受研究方案治疗。患者的中位治疗周期数为4个(IQR:2~6)。
安全性分析显示:最常见的1/2级毒性包括疲劳(11%)、外周神经病变(9%)、腹泻(5%)和脱发(5%);最常见的3/4级毒性包括高血压 (10%)、腹泻 (7%)和外周神经病变(5%)。≥3级的不良事件(AE)及其发生率。
疗效分析:取得部分缓解(PR)、疾病稳定(SD)、疾病进展(PD)和疗效不可评估的患者分别为13例(27%)、26例(54%)、8例(17%)和1例(2%)。
分析患者治疗终止的原因(n=47),分别为疾病进展(n=36)、毒性(n=5)或患者要求(n=1)。1例患者在用药24个周期后,仍在接受治疗。
中位随访7.6个月后,中位PFS和 中位总生存(OS)分别为 4.1个月和 7.8 个月。
目前REPEAT研究尚在进行中的分析包括:瑞戈非尼对紫杉醇药代动力学的影响;对冰冻活检标本进行RNA测序;肿瘤组织中瑞戈非尼作用靶点的免疫组化染色情况。
结论
瑞戈非尼联合紫杉醇80 mg/m2治疗的最大耐受剂量为120 mg/d。这一联合方案于食管胃癌二线或以上治疗的耐受性良好,初步的疗效结果显示了一定的前景,探索性药代动力学和生物标志物终点分析正在进行中。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SMO#
29
#食管胃癌#
29
#ESMO#
37
#食管#
36
#二线治疗#
37
谢谢梅斯提供这么好的信息,学到很多
46