原发性膜性肾病PLA2RAb诊断的10大要点
2018-02-14 MedSci MedSci原创
膜性肾病(MN)是导致肾病综合征的常见原因,亦是终末期肾病的常见原因。 2009年,研究报道70%的原发性MN患者(PMN)抗磷脂酶A2受体抗体(PLA2RAb)阳性,使得我们对该病发病机制的认识取得较大进展。那么,有关PLA2RAb你了解多少呢?1. PLA2RAb的抗原是? 足细胞表面M型磷脂酶A2受体(PLA2R)是PLA2RAb的靶抗原。正常情况下,受体可与PLA2结合,但确切的
膜性肾病(MN)是导致肾病综合征的常见原因,亦是终末期肾病的常见原因。 2009年,研究报道70%的原发性MN患者(PMN)抗磷脂酶A2受体抗体(PLA2RAb)阳性,使得我们对该病发病机制的认识取得较大进展。那么,有关PLA2RAb你了解多少呢?
1. PLA2RAb的抗原是?
足细胞表面M型磷脂酶A2受体(PLA2R)是PLA2RAb的靶抗原。正常情况下,受体可与PLA2结合,但确切的作用机制尚不明确。促使抗体(Ab)产生的因素尚不清楚,但可导致上皮下抗原-抗体复合物沉积,继而激活补体,导致足细胞损伤和蛋白尿。
2. 抗体检测效价是否具有种族差异?
除日本人外(约为50%),不同种族群体的抗体检测率基本相同,无显著差异。儿童PMN的PLA2RAb 检测率为70%。
3. 什么情况下需行肾活检PLA2R检测?
正常情况下,肾活检免疫荧光PLA2R染色呈弱阳性。而PLA2RAb阳性的PMN患者,免疫荧光检查可见PLA2R强阳性,沿毛细血管壁呈颗粒状沉积。病情缓解,PLA2RAb阴性的特发性MN患者,确诊其是否患有PLA2RAb阳性疾病的唯一方法为进行初始肾活检PLA2R染色。部分血清PLA2RAb阴性的患者,肾活检也可显示PLA2R阳性(10%-15%);同PMN一样,患者血清学阳性可早期出现,也可晚期出现。主要原因为,肾脏一开始可代偿,血清学检测可能晚于肾脏病活动度。
4. 不同抗原表位有何联系?
1型PLA2R具有9个不同的结构域,其中胞外胱氨酸富集区(CysR)结构域为主要表位。阻断单个表位是临床的关注热点,但后来发现表位谱可随时间的迁移而变化,其他结构域抗体表达可能与不良预后相关。未来可能实现检测表位特异性PLA2RAb水平,但目前依然是检测的总抗体滴度。
5. PLA2RAb检测的特异性和敏感性如何?
酶联免疫吸附剂测定是检测PLA2RAb水平的常用方法,为抗体阳性定量检测。虽然约2/3的乙肝、丙肝或结节病相关性MN患者也可表现为PLA2RAb阳性,但PLA2RAb检测特异性依然>90%,敏感性为70%。
6. 肾病综合征患者诊断PMN是否可用PLA2RAb阳性代替肾活检?
鉴于其他蛋白尿性肾脏病并不能检测到PLA2RAb,理论上来讲,部分患者可不用进行肾活检。但目前,肾活检依然是确诊的“金标准”。
7. PLA2RAb可用于监测疾病活动度吗?
PLA2RAb滴度是临床上重要的生物标志物(图1)。监测PLA2RAb水平和评估免疫缓解有助于患者避免不必要的免疫治疗。高PLA2RAb水平提示自发缓解的可能性较小,随着时间的推移,抗体水平可进一步增加。疾病复发前约3个月抗体水平升高。
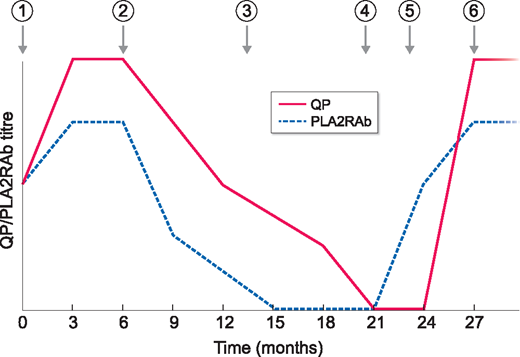
PLA2RAb作为生物标志物在PMN中的意义;QP:定量蛋白尿;时间点:1 =疾病诊断;2 =给予免疫抑制治疗;3 =血清学缓解;4 =蛋白尿缓解;5 =血清学复发;6 =蛋白尿复发
8. PLA2RAb水平是否有助于评估治疗反应?
使用免疫抑制剂后PLA2RAb水平即出现下降。若治疗后PLA2RAb滴度下降未> 50%,提示预后不良。此外,获得临床缓解后PLA2RAb持续阳性提示复发的可能性较大。
9. PLA2Ab水平可预测移植后复发吗?
PMN是移植后复发最常见的肾小球肾炎。研究表明,PLA2RAb阳性预测移植后复发具有较高的阳性预测值。已知PLA2RAb阳性的PMN患者,监测抗体水平具有一定的临床意义,抗体滴度增加或抗体阳性可提示复发。
10.PLA2RAb水平是否会成为临床试验的替代指标?
目前没有任何试验正在以此为基础进行,但未来可能会考虑免疫学缓解(一种更快实现的终点)。
小结
临床上,检测PLA2RAb有助于确诊PMN。作为生物标志物PLA2RAb在监测疾病,检测缓解率或复发方面具有重要意义,并有助于避免不必要的治疗。
原始出处:
McQuarrie EP. Anti-phospholipase A2 receptor antibodies in primary membranous nephropathy-10 key points. Nephrol Dial Transplant. 2018 Feb 1;33(2):212-213
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PLA2#
42
#原发性#
27
这里是真正的完整版的.
58
学习了
61
学习了
61