JCO:晚期非小细胞肺癌抗肿瘤治疗的方案、生存期和花费情况如何?
2017-05-26 石岩 环球医学
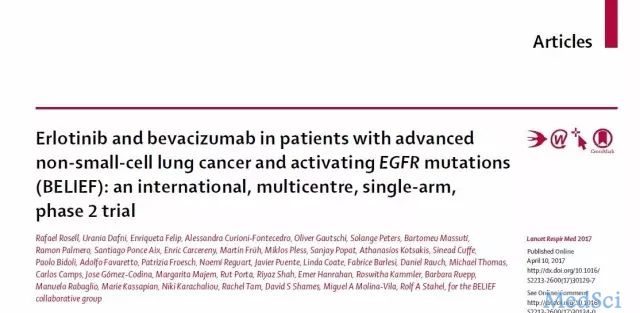
2017年1月,发表在《J Clin Oncol》的一项由美国科学家进行的研究,考察了2000~2011年间晚期非小细胞肺癌(NSCLC)抗肿瘤治疗的治疗方案、生存期和花费。目的:过去十年中,针对NSCLC的多种药物已经得到批准,但有关它们的使用及相关花费和生存期却知之甚少。方法:研究人员使用的SEER-Medicare 2000~2011年间,新确诊为晚期NSCLC并接受抗肿瘤药物治疗的老年患者
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抗肿瘤治疗#
37
#JCO#
25
#非小细胞#
23
#肿瘤治疗#
29
#生存期#
26
期待未来的pd1和car改变这一状况!
53