深度解析盲法桡动脉穿刺
2016-11-25 温州医科大学附属浙江省台州医院麻醉科 丛海涛 MedSci原创
在围术期经常需要血气分析和动脉测压。通常需要进行动脉穿刺置管。桡动脉较易触及,置管后并发症少,是动脉置管首选部位。很多年轻医生在做桡动脉穿刺的时候成功率不是很高,清醒病人甚至难以接受反复穿刺,耗时过长也会影响临床工作,同时年轻医生信心容易受到打击,出现挫折感和为难情绪。在超声下我们可以测量出桡动脉的直径,根据桡动脉粗细我们将动脉分成三类:1.Bad 不好
在围术期经常需要血气分析和动脉测压。通常需要进行动脉穿刺置管。桡动脉较易触及,置管后并发症少,是动脉置管首选部位。很多年轻医生在做桡动脉穿刺的时候成功率不是很高,清醒病人甚至难以接受反复穿刺,耗时过长也会影响临床工作,同时年轻医生信心容易受到打击,出现挫折感和为难情绪。
在超声下我们可以测量出桡动脉的直径,根据桡动脉粗细我们将动脉分成三类:

穿刺难度大的情况包括:老年、女性、肥胖、低血压及血管迂曲、脉搏细速、触摸不清楚等情况。
动脉穿刺置管包括两个步骤:第一步是击中动脉,第二步是置管。对于抽血气采血样来讲第一步即可达到要求,对围术期循环监测来讲需要置管。穿刺失败包括两种情况:第一种情况是击不中动脉,开玩笑的说法是穿了很久连个红细胞都没穿到。第二种情况是击中动脉无法成功置管,出现动脉损伤和血肿。
The first is the best!一针见血!这是我们击中动脉的最理想的情况。如何做到呢?动脉准确定位是关键!
动脉定位有两种方法:第一种方法是用食指去触摸,建议将食指竖起来,指甲不能过长,这样减少接触面积,同时上下移动感受搏动最明显的位置,这样定位范围更小更准确。向近心端移动确定穿刺方向。初学者可以做好穿刺点和穿刺方向的标记。第二种方法是用超声定位:通过超声图像我们可以清晰的看到桡动脉的位置、粗细、距离皮肤的距离,动脉的走形、是否有迂曲痉挛和血栓等。选择容易穿刺的部位做好标记。
为什么动脉穿刺过程中置管会失败?笔者首先通过打靶来解释失败的原因。
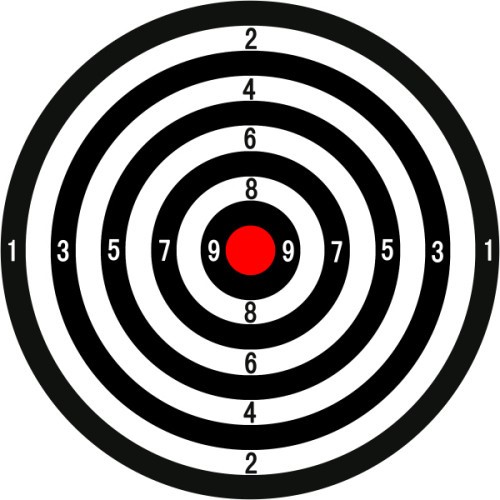
击中动脉如果是在血管壁或靠近动脉壁的地方类似打靶在0环或者1环等较低环数处,不仅针尖容易损伤动脉壁导致血肿甚至动脉夹层,而且动脉损伤后容易形成血栓和动脉痉挛,导致外套管在血管外或直接顶在血管壁上以致难以置入。需要调整才能成功。9环10环即血管的横截面中心位置或附近最理想,置管会非常顺利。
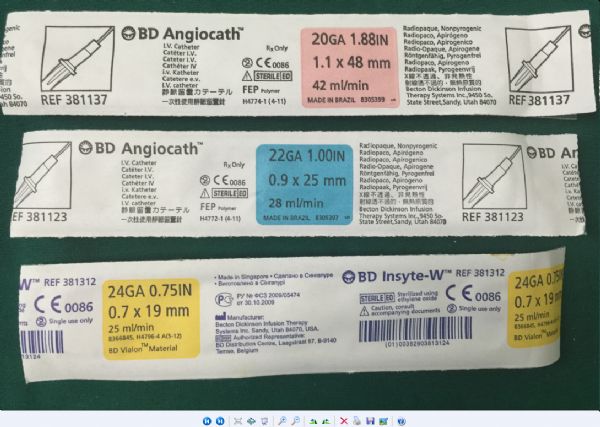
动脉留置针成人(>30kg)选用20G(红),小儿(5~30kg)选用22G(蓝),婴儿(<5kg)选用24G(黄)。
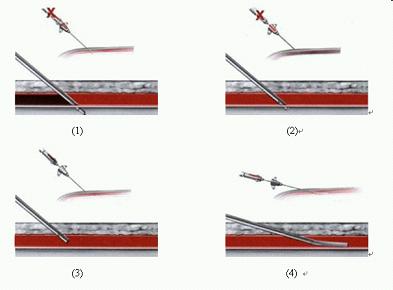
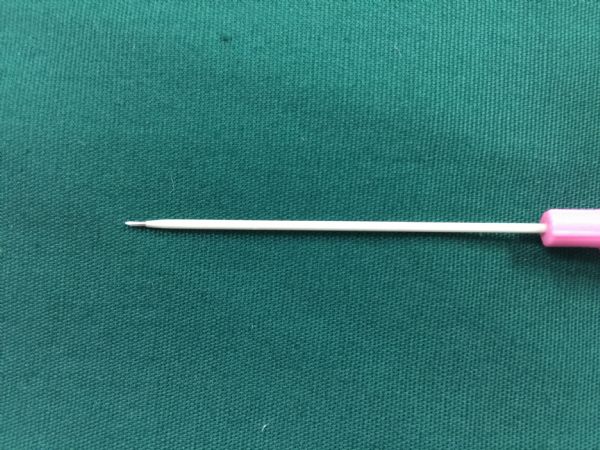
从以上图片我们可以看出成人20G穿刺针的针芯尖和外套管顶部是有2~3mm距离的。因为桡动脉很细,容易出现以下四种情况:
1、针芯尖在桡动脉内而外套管在血管外;
2、针芯尖和外套管均在桡动脉内;
3、针芯尖在血管外而外套管在血管内;
4、针芯尖和外套管均在血管外情况。
最理想的情况是第2种情况针芯尖和外套管均在桡动脉内。第1种情况处理方法就是继续进针,第3种情况处理方法直接退针芯,见套管血流出即可置管,第4种情况要先退出针芯,后退出外套管,见套管血流出即可置管。
对于难以触摸动脉和难以击中动脉情况我们有何策略和方法呢?
当选定了穿刺点后,如果按照自己既定的方向穿刺没有血液从针尾部流出,初学者会反复同一个方向穿刺,完全没有章法,自我感觉明明动脉搏动就在穿刺针的方向。这时可以通过笔者命名的"微调三针法"来微调穿刺方向。向左侧和向右侧略微调整操作方向,如果均未能击中动脉,应该更换穿刺点。再次采用微调三针法直至击中动脉。
为什么不能大幅度调整穿刺方向?如果以大角度调整后击中动脉,针芯很容易处在动脉壁附近位置,相当于打靶打在较低环数位置,外套管和动脉成大角度,置管会出现困难。
在调整穿刺方向时,每次退针一定要退到皮下,否则插入过深一直在动脉的平面以下是不会击中动脉的。可以通过超声来观察自己的进针是否过深来纠正错误的操作习惯。
皮肤松弛的、动脉易滑动的要用食指按压住搏动的动脉,穿刺针击中后见到针尾部有血液流出放松手指,再进行下一步操作。
有些体型偏瘦、血压高的患者,肉眼都能观察到桡动脉搏动,只需触摸近心端搏动点,远近两点一线即为穿刺方向。穿刺多易成功。
对于无法触摸到动脉搏动的患者可选用解剖穿刺法。解剖穿刺法是根据经验选择大概的穿刺点位置,应用微调三针法穿刺,直到穿刺成功。这种情况下更适合应用超声定位。超声是血管穿刺的利器, 看到搏动形态或应用彩色多普勒观察血流,看下PW图像,有动脉波形即可确认动脉。
对于置管困难的情况我们有何策略和方法呢?
穿刺针针芯和外套管有2~3mm的距离,所以针芯进入血管后,看到针芯尾部血液流出不必着急,将针整体放平,再前进放平后继续前行2~3mm,这样做的目的是保证外套管也进入血管内。如果针芯尾部还有血液流出,说明针芯和外套管都在血管内,退出针芯即可置管成功。
如果尾部血液停止流出,可以退出针芯,如果外套管有血液流出,则置管成功。如果无血流流出,再后退外套管,有血液流出则置管可成功。若还是没有血液流出,则可以放回针芯,应用微调三针法,直到针芯见血后再放平置入2~3mm一直有血液流出,置入外套管。重复以上操作步骤直至置管成功。
操作时间过长会导致针尾部很快充满血液无法观察血液流出情况以致无法确认针芯是否在血管内。针尾部充满血液后可以在拔出针芯后在套管尾部接上5ml注射器来判断外套管的位置。注射器好处是可以容纳多余的血,也可以将血液推回动脉内。但不能认为动脉血是抽出来的 一定是快速流出来的。一旦不畅或者缓慢抽出就代表外套管不在血管内,很可能是在血管旁。
在临床工作中初学者可以在抽血气的时候通过置入20G穿刺针导管来抽血样,可以增加操作练习机会。
下面介绍下桡动脉盲探穿刺具体操作流程:
完整的操作具体包括穿刺五要素:穿刺点;穿刺方向;穿刺角度;穿刺深度;穿刺速度。
1、穿刺点的选择
腕横线桡骨茎突旁桡动脉搏动最清楚处;一般选择在桡骨茎突近端1cm处;桡侧腕曲肌肌腱和桡骨头之间;因为该部位桡动脉的走行较直且相对表浅,穿刺容易成功,而且分支相对较少,误入分支血管的几率较小。
2、穿刺的方向
朝着动脉行走向心方向穿刺;向前进针针尾内有鲜红血液回流,表明套管针针芯进入了动脉;适当降低穿刺针与皮肤的角度,再进针2mm,目的是让穿刺针的外套管进入动脉内;
① 如仍有鲜红血液回流,表明套管针完全进入了动脉。略退出针芯,置入外套管;
②如无,退出针芯,出现回流表明虽然针芯穿出动脉内但外套管仍然在动脉内,置入套管针;
③退出针芯,仍无回流表明针芯和外套管都在血管外,将外套管后退,血液回流,置入套管针。
④退出针芯,无回流,退外套管也无回流,表明穿刺失败,重新穿刺。
3、穿刺的角度
套管针与皮肤一般呈30~45°角;针的角度越小,可能穿刺针芯进入动脉的点越靠近近心端,针走的距离越长,但是越容易置管。
4、穿刺的深度
与选择的穿刺点有关,桡骨茎突旁最表浅,皮肤下方即为桡动脉;超声可以明确皮肤到桡动脉的距离;浅的2-3mm,深的可达5-10mm。
5、穿刺的速度
皮肤松弛的、动脉易滑动的可以进针速度快些;
皮肤太紧的的要慢些进针;穿透法一般进针速度较快。
患者常采用仰卧位,左上肢外展于托手架上,穿刺者位于穿刺侧,患者手臂平伸外展20°~30°,手掌朝上,手指指向穿刺者,将塑料小枕放置患者腕部,使腕关节抬高5~8cm,并且保持腕关节处于过伸状态。
穿刺时将穿刺者左手的食指、中指、无名指自穿刺部位由远至近依次轻放于患者桡动脉搏动最强处,指示患者桡动脉的走行方向,食指所指部位即为穿刺的"靶点",穿刺点在桡骨茎突近端0.5cm即第二腕横纹处,感觉动脉搏动。三指所指线路即为进针方向。
穿刺方法可以分为直接穿刺法和穿透法。因穿透法损伤大临床常用直接穿刺法。
1.直接穿刺法
摸准动脉的搏动部位和走向,选好进针点,在局麻下或全麻诱导后用20G留置针进行桡动脉穿刺。
针尖指向与血流方向相反,针体与皮肤夹角根据病人胖瘦程度而异,一般为30°~45°,缓慢进针,当发现针芯有回血时,再向前推进2~3mm,固定针芯,向前推送外套管,后撤出针芯,这时套管尾部应向外搏动性流出,说明穿刺成功。

2. 穿透法
进针点、进针方向和角度同上。当见有回血时再向前推进0.5mm左右,然后撤出针芯,将套管缓慢后退,当出现血液搏动性流出时停止退针,并立即将套管向前推进,送入时无阻力感且血液搏动性流出,说明穿刺成功。
作者介绍
丛海涛,麻醉学硕士,副主任医师,温州医科大学附属浙江省台州医院麻醉科教研室副主任,麻醉科首席医师。负责麻醉科规范化培训工作,浙江省住院医师规范化培训评估与质控专家。温州医科大学兼职讲师。台州市211人才工程培养人员。浙江省神经科学委员会麻醉学分会会员。在国内知名期刊发表多篇论文。曾在中国医学科学院阜外心血管病医院进修心血管麻醉,擅长心胸外科麻醉,疑难危重病人麻醉管理及临床麻醉围术期病人处理。能熟练运用麻醉学专业技术进行各专科麻醉,能熟练应用各种技术进行复杂、重症手术的麻醉管理以及术后危重病人的监测与治疗。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#解析#
31
#桡动脉穿刺#
31
对小年轻作用极大。一下思路清晰了。谢谢老师的分享,?
66
好文!太棒了!
0
心血管科的常规
54
总结的非常全面,剖析非常透彻,从部位、解剖、方法、对策诠释了动脉穿刺技术,大大提高穿刺成功率。
0
#穿刺#
29
#桡动脉#
34
深度解析盲法桡动脉穿刺
52
熟能生巧!
37