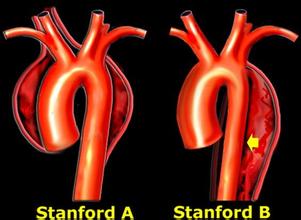
JACC:主动脉夹层患者的血管内修复还是开放手术修复?
2016-11-13 fsy MedSci原创
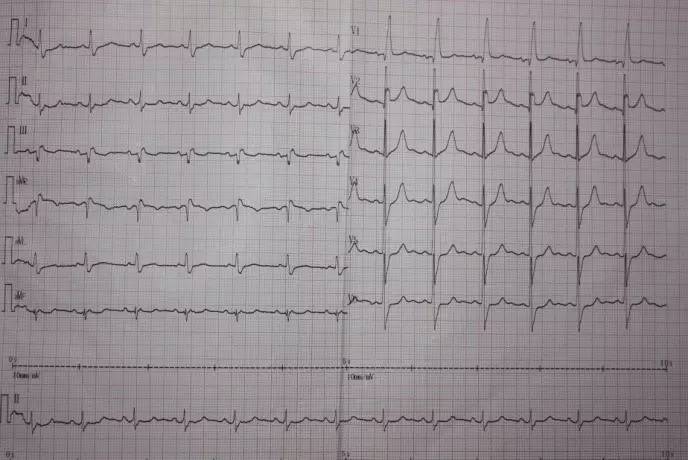
对于无法接受急性主动脉夹层的腔内修复术的患者,支架植入是一种治疗选择。然而,关于预后的随访结果数据是有限的。这项研究报告了主动脉夹层患者血管内修复的中期结果,这些患者被认为接受开放修复手术的风险较高。在2009年5月1日至2011年1月31日期间,来自中国的研究人员安排15例不符合直接手术修复的主动脉夹层患者(45〜78岁)接受血管内修复(1例急性夹层,7例亚急性夹层和7例慢性夹层),平均随访时间
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
32
#手术修复#
42
#开放手术#
35
#ACC#
40
#主动脉#
33
#动脉夹层#
25