重磅!2016中国成人血脂异常防治指南更新要点解析
2016-10-25 复旦大学附属华山医院 李勇 中国医学论坛报
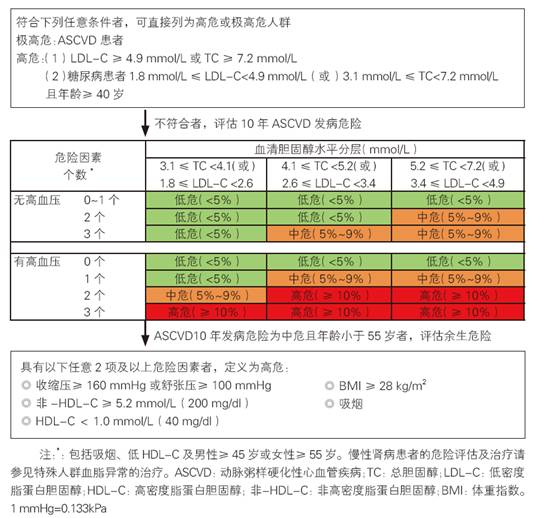
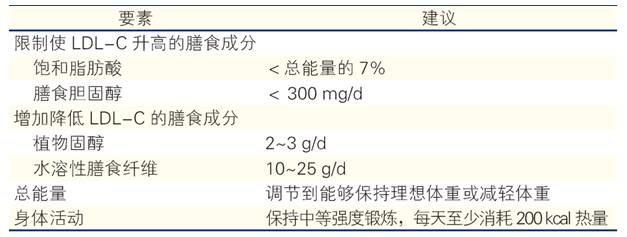
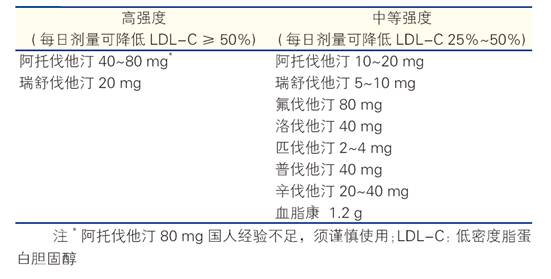
最新一版的《中国成人血脂异常防治指南》已于2016年10月24日正式发布,距2007年发布的上一版指南已接近十年。近十年间,血脂领域无论在循证证据还是在药物研发方面均有进一步更新。在诸骏仁教授和高润霖教授领导下,指南制定专家组以我国流行病学数据及随机对照研究证据为基础,结合我国真实世界临床实践的国情,同时参考国际指南的变迁,修订工作参考了世界卫生组织、中华医学会临床指南制定的标准流程,在指南修


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#指南更新#
22
#解析#
23
#防治指南#
26
#血脂异常#
23
#重磅#
30
学习了,赞一个!!!
66