Blood:免疫调节剂通过降解CK1α、下调IRF4表达来杀伤原发性积液性淋巴瘤细胞!
2018-07-02 MedSci MedSci原创
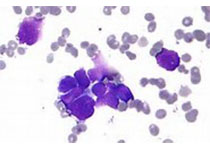
原发性积液性淋巴瘤(PEL)是一种侵袭性肿瘤,治疗方式有限。近期研究人员发现免疫调节剂(IMiDs)来那度胺和泊马度胺可杀伤PEL细胞,现有临床试验正在研究用那度胺治疗PEL。IMiDs与CRL4[CRBN]E3泛素连接酶复合物结合,使其捕获Ikaros家族锌指蛋白1和3(IKZF1和IKZF3)、酪蛋白激酶1α(CK1α)和锌指蛋白91(ZFP91)作为底物。IMiDs可有效治疗多发性骨髓瘤,主
IMiDs与CRL4[CRBN]E3泛素连接酶复合物结合,使其捕获Ikaros家族锌指蛋白1和3(IKZF1和IKZF3)、酪蛋白激酶1α(CK1α)和锌指蛋白91(ZFP91)作为底物。IMiDs可有效治疗多发性骨髓瘤,主要机制是通过降解IKZF1和IKZF3,进而抑制干扰素调节因子4(IRF4)和MYC的表达。此外,来那度胺还可有效治疗染色体5q缺失相关的骨髓增生异常综合征,机制是通过促进CK1α降解。
近期,有研究人员提出一个基本的IKZF1-IRF4-MYC轴来解释IMiDs对于PEL细胞产生的毒性作用。
在本研究中,Ajinkya Patil等人利用CRISPR/Case9在全基因组范围内筛选至关重要的人类基因,对IMiD作用于PEL细胞系的效应进行深入研究。通过筛查和大量验证实验显示在IKZF1、IKZF3、CK1α和ZFP91四种底物中,仅CK1α对PEL细胞系的存活至关重要。与此相反,IKZF1和IKZF3可有可无。此外,IRF4在8个受检测的PEL细胞系中都至关重要,IMiDs可独立于IKZF1和IKZF3之外触发IRF4的表达下调。
CK1α和/或IRF4再表达可在一定程度上抵消IMiD介导的对PEL细胞系的毒性作用。
总而言之,IMiD作用于PEL细胞的毒性作用不依赖IKZF1和IKZF3,而是通过介导降解底物CK1α和下调IRF4的表达来发挥作用。
原始出处:
Ajinkya Patil, Mark Manzano, and Eva Gottwein. CK1α and IRF4 are essential and independent effectors of immunomodulatory drugs in primary effusion lymphoma. Blood 2018 :blood-2018-01-828418; doi: https://doi.org/10.1182/blood-2018-01-828418
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#原发性#
33
#IRF4#
43
#CK1α#
21
学习了长知识
52
学习了长知识
60
学习了长知识
46