Communications Biology:嵌合体ARCC-4靶向蛋白酶水解作用引起的雄激素受体降解要比恩杂鲁胺效果更好
2018-08-09 AlexYang MedSci原创
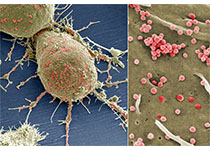
雄激素受体是前列腺癌的一种主要驱使因子,利用竞争性拮抗剂对其转录活性的抑制,比如恩杂鲁胺,仍旧是前列腺癌治疗的一线疗法。然而,大多数的患者最终均发展出药物抗性。最近,有研究人员认为通过蛋白酶水解靶向嵌合体(PROTACs)来以雄激素受体为靶标使其降解,将会成为前列腺癌细胞中靶向雄激素受体信号疗法的一种更好的治疗性策略。研究人员在由一个当前批准的雄激素受体拮抗剂恩杂鲁胺和它的PROTAC衍生物ARC
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#嵌合体#
36
#蛋白酶#
42
#Bio#
29
#RCC#
38
#Biol#
43
#COMMUN#
22
学习了谢谢
71
#雄激素受体#
35
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
51
不错的文章值得拥有哦
58