2018年WCLC:Durvalumab有助于维持无法切除的III期非小细胞肺癌的PFS
2018-09-27 MedSci MedSci原创
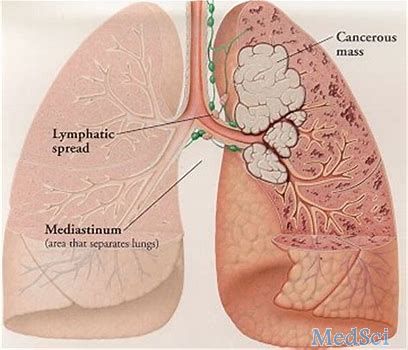
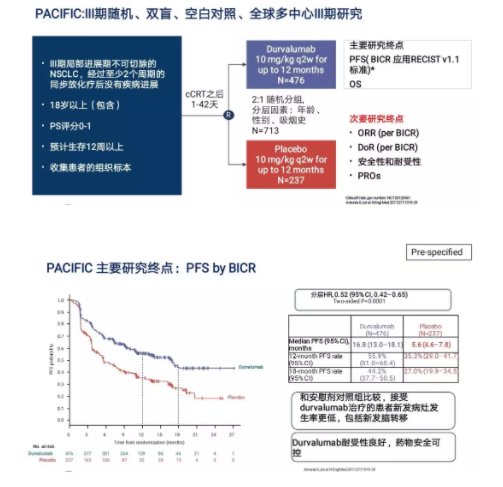
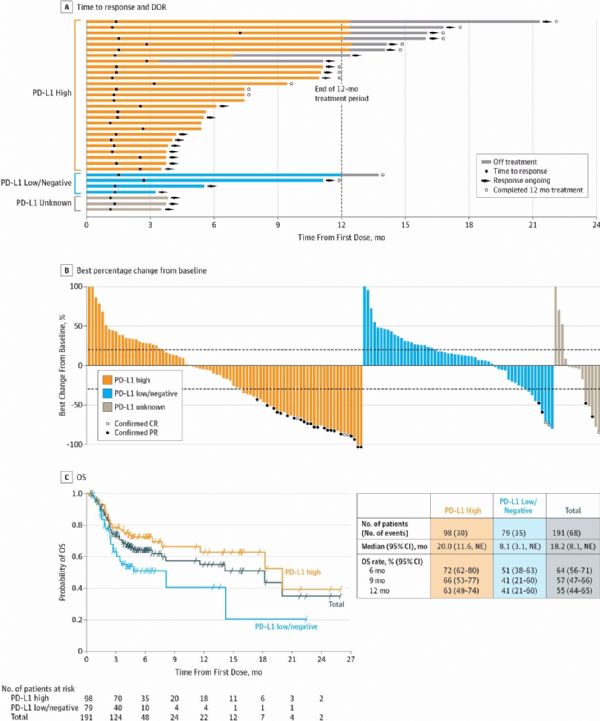
在第19届世界肺癌大会(WCLC)上,III期PACIFIC试验的中期结果显示,在完成标准化放疗后,使用单克隆抗体durvalumab进行维持性免疫治疗,无法切除的III期非小细胞肺癌(NSCLC)患者能够获得更长的无进展生存期(PFS)。
在第19届世界肺癌大会(WCLC)上,III期PACIFIC试验的中期结果显示,在完成标准化放疗后,使用单克隆抗体durvalumab进行维持性免疫治疗,无法切除的III期非小细胞肺癌(NSCLC)患者能够获得更长的无进展生存期(PFS)。
医学博士H. Lee Moffitt称:“与安慰剂相比,durvalumab维持治疗的OS的改善具有统计学意义和临床意义。经durvalumab治疗的患者在无进展生存期、死亡时间、远处转移以及新病灶的发生方面都有所改善”。无法切除的III期NSCLC的护理标准是基于铂的化学放射治疗,然而标准护理治疗的结果很差,只有约15%至30%的患者在5年时仍然存活。
III期PACIFIC试验随机分组了713名患有无法切除的III期NSCLC患者,这些患者在接受铂类放化疗后接受durvalumab(每2周10 mg / kg,最长12个月,n = 476)或相同剂量的安慰剂治疗(n = 237)。主要终点是PFS和OS,关键的次要终点包括转移性疾病或死亡时间、客观反应率、反应持续时间、转移性疾病的中位时间和安全性。
原始出处:
http://www.firstwordpharma.com/node/1593572#axzz5SJBcSQbc
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#III#
32
#mAb#
28
#非小细胞#
30
#WCLC#
0
#PFS#
36
#III期#
28
学习了
63