指南共识|慢性乙型肝炎患者如何停药、停药后如何复查——APASL指导意见
2022-02-10 临床肝胆病杂志 临床肝胆病杂志
在确定CHB患者能否停用NUC的临床标准、停药策略、预测病毒学和生化学复发的临床指标、随访策略、再治疗的标准等均需要进一步的研究,以更好地完善NUC停药指导意见。
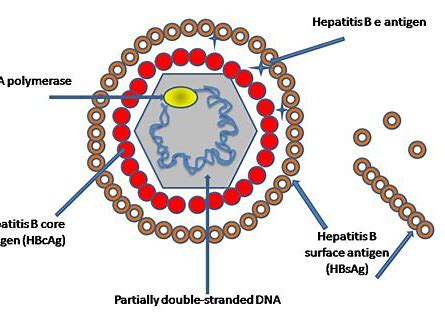
HBV感染目前无法完全根治,强效、安全的核苷(酸)类似物(NUC)长期治疗可通过显著抑制病毒复制,减少肝硬化及相关并发症和肝细胞癌(HCC)的发生,但长期治疗有利有弊。由于NUC抑制病毒作用强、口服方便、耐受性好、不良反应少且轻微等优点,临床应用普遍。但NUC不能完全清除肝细胞内共价闭合环状DNA(cccDNA),难以获得HBsAg清除,HBsAg年转阴率仅为0.15%~0.33%。停用NUC导致病毒学复发和转氨酶升高,继而增加了肝功能失代偿、纤维化进展、HCC或肝病相关死亡的发生风险。亚太肝病学会(APASL)NUC停药指导意见提出了慢性乙型肝炎(CHB)患者的NUC停药标准和后续随访策略,以使停药后获得更好的预后。
1.CHB患者停用NUC的临床标准
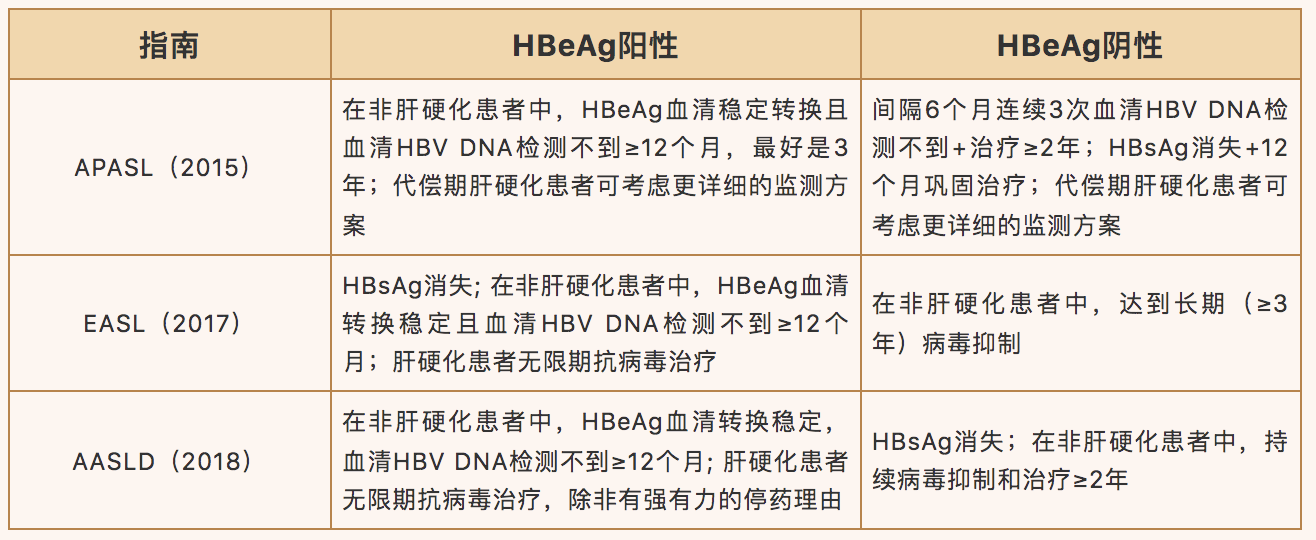
表1比较了APASL、欧洲肝病学会(EASL)和美国肝病学会(AASLD)三大学会指南建议的NUC治疗时间。对于无肝硬化的患者,三份指南均表明,当HBeAg阳性的CHB患者实现HBeAg血清学转换和HBV DNA完全检测不到后至少12个月时,可以停止NUC巩固治疗。
这些指南之间的主要差异在于HBeAg阴性CHB患者停用NUC的时间:APASL指南要求在间隔6个月、连续3次检测不到血清HBV DNA的情况下,治疗≥2年后可停用NUC;EASL指南建议血清HBV DNA检测不到≥3年可考虑停药;AASLD指南则无明确的停药时间建议,以HBsAg清除为治疗终点。
对肝硬化患者而言,仅APASL指南提出了代偿期肝硬化这一特定人群的停药标准,建议通过密切的随访可以考虑停药,而其他指南均提出了无限期治疗。产生上述分歧的原因是不同疾病状态和患者特征导致疾病复杂性不同,进而导致各大指南无法统一。在临床实践中应当结合患者自身情况进行个体化处理。
表1. 三大指南对于CHB患者接受NUC治疗的停药标准
2. NUC治疗有限疗程的优势
2.1 耐药性及长期治疗的安全性
目前各个指南均推荐强效低耐药的NUC,包括恩替卡韦(ETV)、富马酸替诺福韦二吡呋酯(TDF)和富马酸丙酚替诺福韦(TAF),作为一线抗病毒治疗药物,以此减少耐药的发生,但是以下耐药株的出现可能会增加肝癌发生风险:rtA181T/sW172*和rtM204I/sW196*。
NUC的肾毒性罕见,但可能发生在合并高血压、慢性肾脏病或糖尿病的高危患者中。TDF还可能引起骨密度降低和低磷血症,EASL指南建议在高风险人群中将ETV及TAF作为首选。但NUC治疗超过10年的安全性仍未知。
2.2 依从性、长期治疗意愿、经济成本
患者的依从性、长期治疗意愿、经济成本与长期治疗期间的不良结局相关。多项临床研究提示,随着治疗时间的延长,患者的依从性显著下降。长期治疗意愿低或对药物经济成本承担能力低的患者,在长期治疗期间可能发生自行停药或失访。
2.3 NUC停药后的持久性与安全性
依据APASL指南,病毒学复发(VR)定义为HBV DNA从低于检测下限到>2000 IU/mL;而临床复发(CR)定义为伴随着VR的出现,ALT高于2倍正常值上限(upper limit of normal,ULN)。在此基础上,一项最新的系统回顾纳入25项研究,总计1716例患者停止NUC治疗后随访1年,结果显示病毒学应答率仅为51.4%,而持久的生化学累积应答率仅为65.4%。值得注意的是,从安全性角度而言,停止NUC的主要问题是HCC或肝功能失代偿的风险。我国台湾的独立队列研究显示,NUC停药组和长期治疗组的肝硬化患者HCC累积发生率相当,即使根据治疗前特征进行倾向性评分匹配后亦是如此。
2.4 停用NUC后增加HBsAg转阴率
对于HBsAg水平相对较低(尤其是<100 U/mL)的HBeAg阴性患者,停用NUC可能是诱导停止治疗后HBsAg消失的无限期治疗的替代方案。研究显示,在NUC停药后持续应答的患者中,HBsAg降低或转阴最多,在复发但未再治疗的患者中HBsAg降低或转阴较少,在复发并再治疗的患者中HBsAg降低或转阴最少。
这种现象可能是由于抗病毒治疗长期抑制病毒使T淋巴细胞功能恢复,可能导致有效的HBV特异性T淋巴细胞和自然杀伤细胞应答,以应对病毒抗原血症再发。因此,研究对复发患者再治疗的最佳时机和策略非常重要,这样才能既不影响病毒的免疫清除,又能确保患者的安全性。
3.NUC长期治疗的推荐意见
3.1 NUC长期治疗的优势
病毒复制是肝损伤和疾病进展的主要驱动因素,当获得对HBV复制的长期抑制时,疾病进展和肝功能失代偿的风险就会降低。长期NUC治疗可以改善肝脏组织学(坏死和纤维化),甚至可能逆转已存在的肝纤维化或肝硬化,预防或延缓疾病进展,提高HBV相关肝病患者(包括肝硬化﹑失代偿期肝病以及慢加急性肝衰竭)的生存率。研究显示,长期NUC治疗可通过持续抑制HBV DNA恢复HBV特异性T淋巴细胞功能,使得cccDNA以及HBsAg显著下降。因此在长期NUC治疗的基础上序贯或联合应用聚乙二醇干扰素α(PEG-IFNα)可持续抑制HBV DNA,恢复患者细胞免疫功能从而获得HBsAg清除。
3.2 停止NUC治疗的风险
许多研究探索了HBeAg阳性或阴性CHB患者停止NUC治疗的最佳时机及安全性。一项单中心队列研究纳入132例接受NUC治疗的HBeAg阳性CHB患者,42例受试者中,有9例(21%)在HBeAg血清学转换后至少6个月的巩固治疗后停止了NUC治疗,只有2例患者在停药后有持久的病毒学及血清学应答,这表明在大多数CHB患者中,NUC诱导HBeAg血清学转换是暂时的,无论是否发生HBeAg血清学转换,长期NUC巩固治疗似乎是必要的。
比利时的一项队列研究显示,62例HBeAg阳性CHB患者在NUC治疗获得HBeAg血清学转换后,巩固6个月以上停止NUC治疗,其中有30例出现复发,停止NUC治疗导致2例患者因肝脏相关疾病死亡。
一项我国香港的研究显示184例患者接受ETV治疗3年,停药1年的病毒学复发率为91.4%,其中71.8%发生在第24周,治疗前HBeAg阳性的患者获得HBeAg转换后停药复发率显著低于治疗前HBeAg阴性患者的病毒学复发率。
一项对342例我国台湾患者的研究表明,停用TDF的患者比停用ETV的患者病毒学和临床复发率显著升高,并且TDF治疗组临床复发往往更为严重。
一项研究计算出TDF治疗与巩固治疗的最佳持续时间分别为144周和108周。
3.3 联合干扰素的治疗策略有助于NUC安全停药
一项对252例ETV治疗患者的回顾性研究表明,在HBeAg阳性患者中,年龄≥40岁和治疗结束时(EOT)HBsAg水平≥1000 IU/mL的患者停药后的复发风险增加。在HBeAg阴性患者中,同时满足年龄<55岁和EOT时HBsAg水平<150 IU/mL,其VR显著下降,这可能是指导HBeAg阴性患者停止NUC治疗的替代指标。荟萃分析表明,当EOT的HBsAg<100 IU/mL时,无论初始HBeAg状态如何,停药12个月的VR在9.1%~19.6%,而且HBeAg阴性患者停药后39个月的HBsAg清除率为21.1%~58.8%。因此,APASL NUC停药指导意见提出了选择合适的患者实施从NUC转换为或在NUC基础上加用PEG-IFNα治疗来持续降低HBsAg滴度的策略,逐步达到HBsAg消失的“功能性治愈”,以实现NUC安全停药。
对于HBsAg<3000 IU/mL的NUC治疗患者,加用PEG-IFNα治疗可提高HBsAg转阴率,并允许更多患者停止NUC治疗。对于HBsAg水平相对较低(尤其是<100 IU/mL)的HBeAg阴性患者,停用NUC可能是诱导停止治疗后HBsAg消失的无限期治疗的替代方案。对于HBsAg≥3000 IU/mL的患者,继续NUC治疗可能是更好的选择。对于符合NUC停药标准的患者,NUC停药后仍有较高的概率出现VR或临床复发。
4.预测病毒学和生化学复发临床指标
复发预测指标是对停药标准的重要补充,可避免虽符合NUC停药标准但仍有较高复发风险的患者停药。较长的持续治疗时间,尤其是较长的巩固期将降低复发风险。最佳巩固治疗时间仍不确定,不同指南为1~3年。此外,TDF停药后的复发时间显著早于ETV停药后患者。基线血清HBV DNA<2 × 105 IU/mL可预测NUC停药后的持续应答。从开始治疗到血清HBV DNA检测不到的持续时间短于12周,预示着HBsAg血清清除。NUC停药后1个月,血清HBV DNA载量的快速出现可作为未来VR或CR的快速预测因子。
APASL NUC停药指导意见还列举了其他的预测标志物。有新的数据表明,在停止治疗时较低的乙型肝炎核心相关抗原(HBcrAg)、HBV RNA水平与疾病复发显著减少相关,而抗-HBc<100 U/mL有较高的复发风险。
4.1 HBcrAg
有研究探索了EOT时HBcrAg是否与不同临床结局相关。有研究表明,较高的HBcrAg水平与临床复发风险增加相关,每增加1 log U/mL时风险比(HR)增加1.48(95%CI:1.20~1.83)(P<0.0001)。然而,来自中国香港的数据显示,在114例EOT时HBsAg水平<200 IU/mL的ETV治疗患者中,EOT时HBcrAg水平与病毒学复发无关。
总之,HBcrAg能否作为确定NUC停药的良好指标仍不确定,尤其是它如何补充HBsAg来预测临床或病毒复发的,需要进一步研究。
4.2 HBV RNA
血清HBV RNA是HBV复制的另一种潜在标志物,即使在NUC治疗后也可检测到。有学者收集了33例接受不同NUC方案的CHB患者,发现在EOT时可检测到HBV RNA的21例(63.6%)患者的病毒学复发风险更高。另有研究显示,治疗5年后,纳入的23例患者中仅17%可检测到HBV RNA。EOT时可检测到HBV RNA的所有患者均发生重度肝炎复发。最近的一项研究显示,HBV RNA水平与病毒学复发呈正相关,在EOT时HBsAg<200 IU/mL的114例ETV治疗患者中,与HBV RNA低水平的患者相比,HBV RNA≥44.6 U/mL与病毒学复发风险增加相关,HR为2.96(95%CI:1.78~4.93)。
4.3 抗-HBc
较低的抗-HBc水平(<100 U/mL)与较高的临床复发风险可能相关。有研究入组了82例接受ETV治疗的患者,3例患者的抗-HBc<100 U/mL,3例患者在停用NUC后均迅速出现临床复发。有研究入组了100例接受不同NUC治疗方案的患者,在13例抗-HBc<100 U/mL的患者中,随访4年后临床复发达到85%。然而,一项前瞻性队列研究入组了100例接受ETV或TDF治疗的患者,其数据不支持这种相关性。
由于结果相互矛盾,需要更多的数据来证实抗-HBc在指导NUC停药中的临床作用。
5.CHB患者停用NUC后应密切随访
停药后规范随访对于减少疾病复发时肝衰竭的发生非常重要。随访是否有效取决于检测HBV DNA和肝功能的频率。
APASL NUC停药指导意见建议:对于已停药的HBeAg阳性和HBeAg阴性患者,至少在12个月之内,应每1~3个月检测1次。达到HBeAg血清学转换的患者停用NUC后,病毒学和生化学复发的概率低于HBeAg阴性患者。因此,此类患者停药后的随访可相对宽松。同时应每3~6个月复查HBeAg,因有数据提示部分患者可从抗-HBe阳性逆转为HBeAg阳性。治疗前HBeAg阴性患者在停药后应密切随访。由于停用NUC(ETV除外)后前3个月内复发率较高,因此,建议在停药最初3个月内每个月复查ALT和HBV DNA,此后至少每3个月复查1次直到1年。鉴于ETV治疗患者停药后复发较晚,可在ETV停药6个月之后开始强化随访。随访的目的在于早期发现生化学复发或临床复发,重新开始治疗以预防肝功能失代偿或肝衰竭。
最后,CHB患者停用NUC其实是一个包括停药前评估、实施停药、预测复发、停药后随访和停药后再治疗等多个阶段的动态综合诊疗过程。目前各CHB防治指南所推荐的停药标准仍存在一定的局限性。对于有高复发风险的患者,仍然需要延长巩固疗程或者长期服药,以避免出现停药后复发,导致肝病进展、暴发性肝衰竭甚至死亡。未来,在确定CHB患者能否停用NUC的临床标准、停药策略、预测病毒学和生化学复发的临床指标、随访策略、再治疗的标准等均需要进一步的研究,以更好地完善NUC停药指导意见。
原始出处
任姗, 郑素军. 《2021年亚太肝病学会慢性乙型肝炎患者停用核苷(酸)类似物指导意见》摘译[J]. 临床肝胆病杂志, 2022, 38(1): 78-80.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#乙型肝炎#
55
#指导意见#
51
#肝炎患者#
55
#慢性乙型肝炎#
54
#APA#
43
#停药#
39
#ASL#
41
#APASL#
45