Diabetes Care:2型糖尿病中磺脲类药物对心脏线粒体KATP通道的特异性与主要不良心血管事件风险的关系
2022-08-22 从医路漫漫 MedSci原创
SUR除存在于胰岛β细胞外, 还见于其他组织, 如心脏、血管、脑等。
背景:作为控制血糖的主要药物, SU是否会增加心血管事件的风险一直倍受争议。早在1971年, 美国大学团体糖尿病计划 (UGDP) 试验发现甲苯磺丁脲会增加患者心血管事件和全因死亡, 之后甲苯磺丁脲退出市场。但迄今为止, 其他SU并未被明确证实会增加心血管事件及其病死率。SUR除存在于胰岛β细胞外, 还见于其他组织, 如心脏、血管、脑等。心血管系统的SUR激活可能存在双向影响:某些SU能够关闭心血管系统ATP敏感性钾通道, 增高冠脉张力, 加重缺血对心血管组织的损伤和促进心脏肥厚的发生;另一方面, SU能够激活过氧化物酶体增殖物激活受体、调控糖脂代谢、抑制炎症反应和延缓动脉粥样硬化的发生。此外, 不同SU剂量对胰岛β 细胞上SUR1 以及心肌细胞SUR2A和血管平滑肌细胞SUR2B的作用可能存在差别。因此, 不同受体特异性的SU心血管安全性可能也存在不同。
目的:先前的研究已经揭示了磺酰脲类药物在主要不良心血管事件(MACE)的不同类别。体外和体外研究报道了几种磺脲类药物对心脏线粒体钾敏感ATP(mitoKATP)通道表现出高亲和力阻断,并可能干扰缺血预适应,这是自我心脏保护的最重要机制。然而,还没有研究证实磺酰脲类化合物的这些不同的结合亲和力是否可以解释它们在MACE中的内部差异。我们比较了mitoKATP通道高亲和力和低亲和力磺酰脲类药物在现实环境中的MACE风险。
研究设计与方法:利用台湾全国医疗保健索赔数据库,将2007 - 2016年期间开始磺酰脲类单药治疗的2型糖尿病患者纳入队列研究。预测因子包括年龄、性别、首次糖尿病诊断到首次使用磺脲类药物的时间、进入年份、糖尿病严重程度代理指标、医生就诊次数、住院次数、以月收入为基础的保险费和医院水平,所有这些都是在启动磺酰脲类药物之前的前一年测量的。在1:1倾向评分匹配后,共有33,727个新的mitoKATP通道高亲和力(格列本脲和格列吡嗪)和低亲和力(格列齐特和格列美脲)磺酰脲使用者被确定。Cox比例风险模型用于估计调整后的风险比(aHRs)和95% CI。
结果:MitoKATP通道高亲和力磺酰脲类药物与三点MACE (aHR 1.21 [95% CI 1.03-1.44])、缺血性卒中(aHR 1.23 [95% CI 1.02-1.50])和心血管死亡(aHR 2.61 [95% CI 1.31-5.20])风险显著增加相关,但与心肌梗死(aHR 1.04 [95% CI 0.75-1.46])风险无关。持续时间-反应分析显示,治疗90天内发生MACE的风险最高(aHR 4.67 [95% CI 3.61-6.06])。
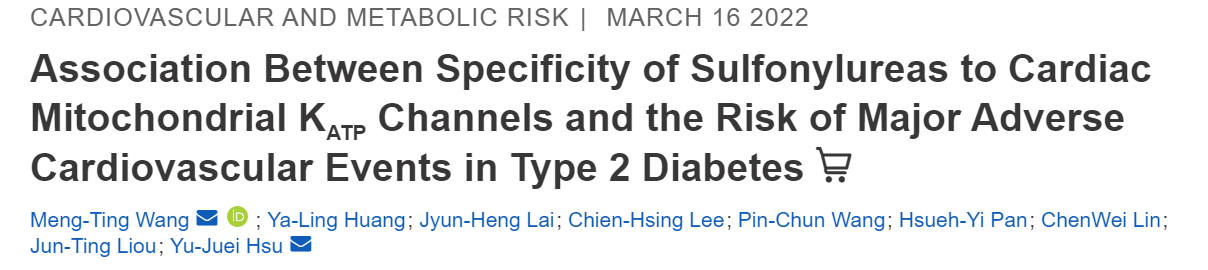
表1 随访期间线粒体KATP通道的平均持续时间和截断原因-高亲和力磺酰脲单药治疗和低亲和力磺酰脲单药治疗的结果

表2 随访期间线粒体KATP通道-高亲和力磺酰脲单药和低亲和力磺酰脲单药治疗的平均持续时间和截断原因,按结果分析(续)
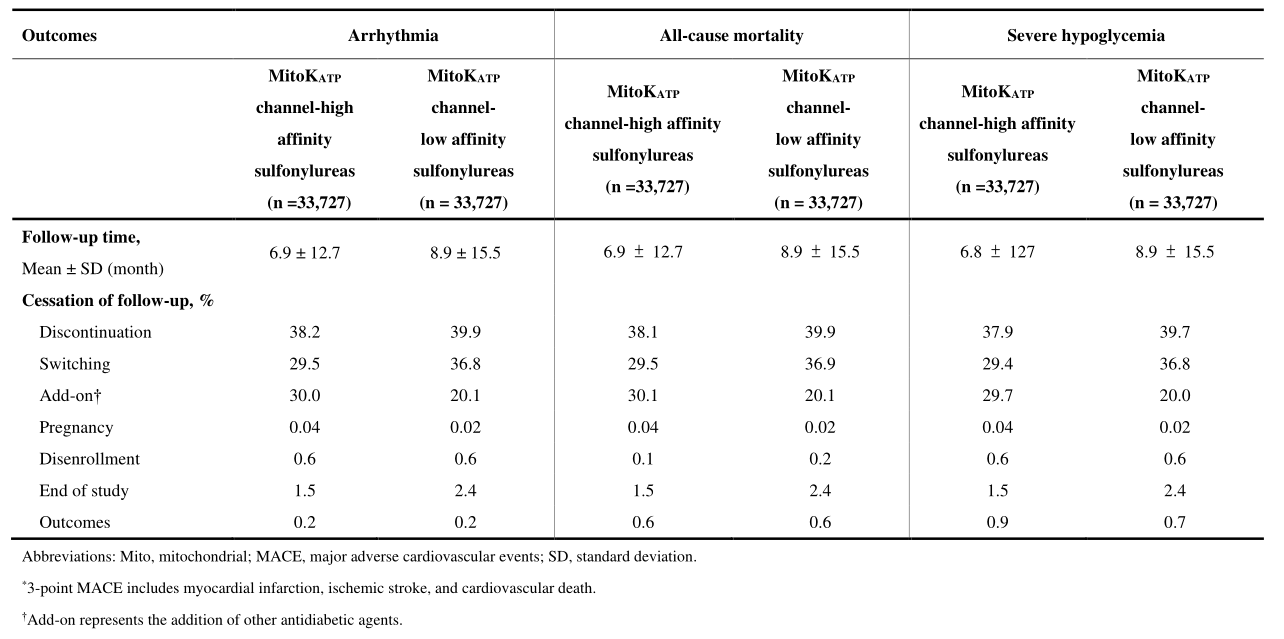

图1 线粒体KATP通道-高亲和力磺酰脲单药组与线粒体KATP通道-低亲和力磺酰脲单药组患者的三点主要不良心血管事件(A)、心肌梗死(B)、缺血性卒中(C)、心血管死亡(D) Kaplan-Meier生存曲线
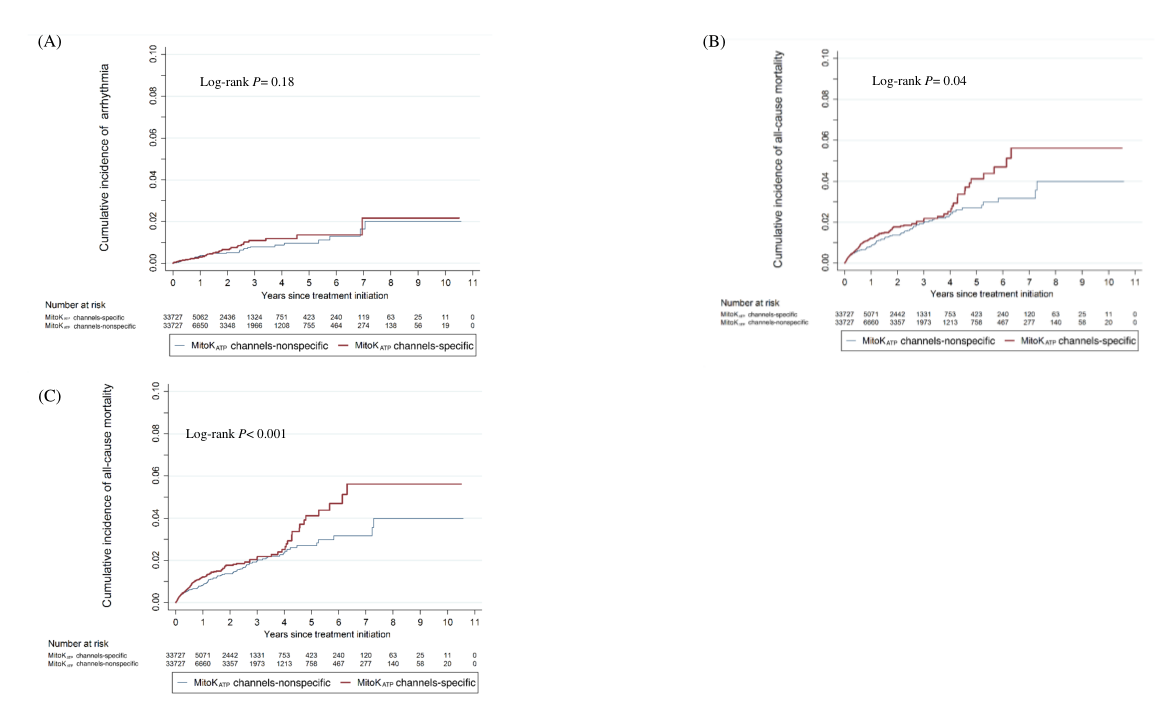
图2 线粒体KATP通道-高亲和力磺酰脲单药组和线粒体KATP通道-低亲和力磺酰脲单药组患者心律失常(A)、全因死亡率(B)和严重低血糖(C)的Kaplan-Meier生存曲线
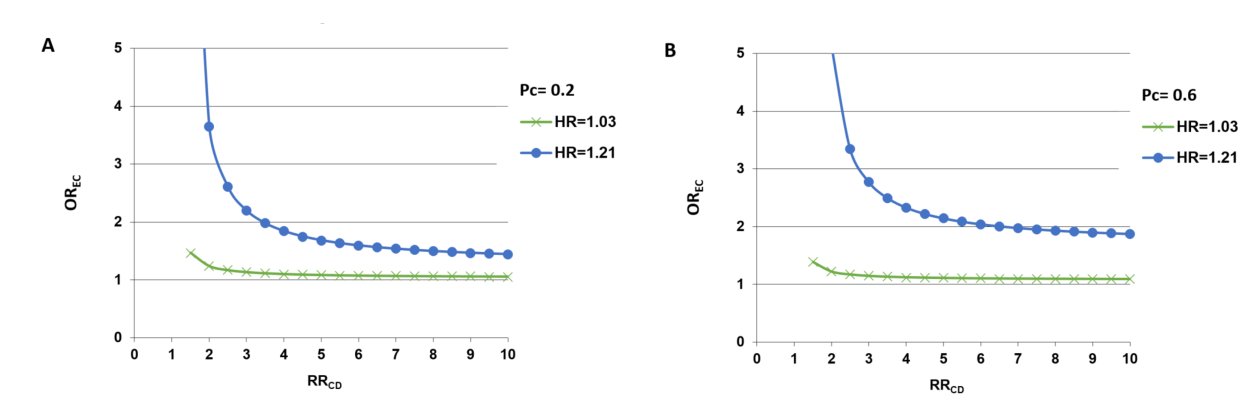
图3 采用排除方法来评估未测量的混淆对主要发现的影响
结论:在全国糖尿病人群中,心肌mitoKATP通道高亲和力磺酰脲类药物与低亲和力磺酰脲类药物相比,与MACE风险增加相关。

原文出处:
1.高慧,沈云峰,赖晓阳.磺脲类药物安全性研究进展[J].南昌大学学报(医学版),2012,52(11):101-103+10
2.Wang MT, Huang YL, Lai JH,et al.Association Between Specificity of Sulfonylureas to Cardiac Mitochondrial KATP Channels and the Risk of Major Adverse Cardiovascular Events in Type 2 Diabetes.Diabetes Care 2022 05 01;45(5)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Diabetes#
45
#DIA#
63
#BET#
41
#特异性#
64
#风险的关系#
0
#血管事件#
41
#心血管事件风险#
44
#磺脲类#
41
#ATP#
49
#主要不良心血管事件#
42