Nat Commun:开发靶向FZD/SMO抗癌药物新思路!
2019-02-14 Ruthy 转化医学网
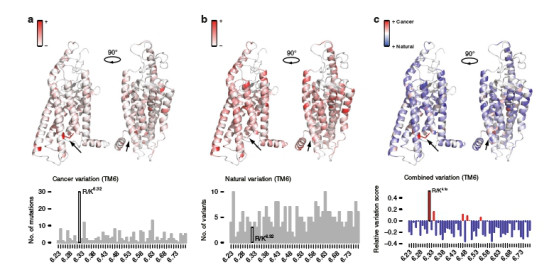
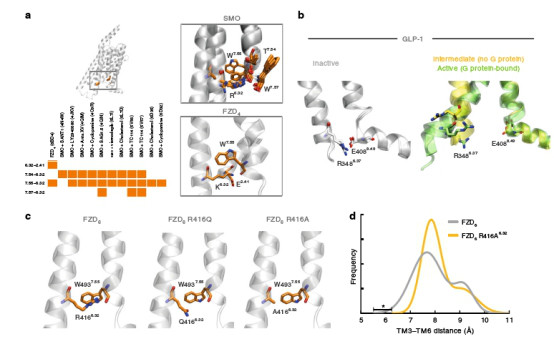
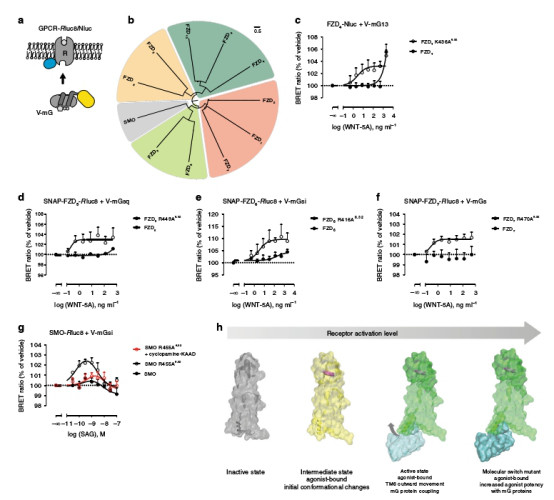
G蛋白偶联受体(GPCRs)是人体内最大的膜受体蛋白家族,其介导的信号通路已经被证明是原癌基因信号的关键调控者,而GPCRs则是很好的药物靶点。但有研究证实F类GPCRs(FZD/ SMO)具有结构保守性,其在受体激活后的结构变化始终难以盖棺定论,导致靶向FZD/ SMO的抗癌药物研究停滞不前。近日,卡罗林斯卡研究所的研究人员发现一种特殊的氨基酸——受体跨膜区TM6/7间的接触网可作为介导FZD/
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SMO#
0
#新思路#
33
#Nat#
50
#COMMUN#
26
#抗癌药物#
29
#抗癌药#
27