Lancet Oncol:奥拉帕利联合阿比特龙治疗转移性去势抵抗性前列腺癌的患者报告的预后
2022-09-09 MedSci原创 MedSci原创
奥拉帕利与阿比特龙联合使用可显著延长转移性去势抵抗性前列腺癌患者的影像学无进展生存期,且不会影响期生活质量
前列腺癌是全球男性第二产检的癌症,是男性癌症相关死亡的第五大原因。在未筛查人群中,约14%的患者确诊时已发生转移,高达40%的未转移患者即使接受积极治疗最终也会转移。
一项双盲的2期试验显示,转移性、去势抵抗性前列腺癌患者采用奥拉帕利联合阿比特龙相比安慰剂联合阿比特龙治疗可获得显著更长的无进展生存期。本文报告了该试验的探索性分析结果:患者报告的疼痛和健康相关生活质量(HRQOL)。
该研究是一项在欧洲和南美洲的11个国家联合开展的双盲、随机、安慰剂为对照的2期试验,受试患者是年满18岁的转移性、去势抵抗性、既往接受过多西他赛治疗的前列腺癌患者,1:1随机接受口服奥拉帕利(300 mg*2次/天)或安慰剂+口服阿比特龙(1000 mg/天)和口服强的松或泼尼松龙(5 mg*2次/天)治疗。主要终点是影像学无进展生存期(已报道)。探索性终点是患者报告的预后:HRQOL。
2014年11月25日至2015年7月14日,共筛查了171位患者,其中29位被排除。142位患者被随机分至两组(每组各71位)。截止2017年9月22日,奥拉帕利组和安慰剂组分别中位随访了15.9个月和24.5个月。问卷依从性普遍较高(43-100%)。
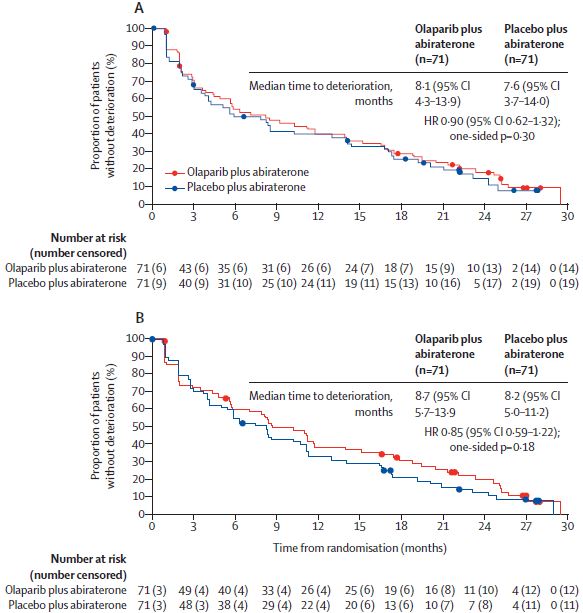
两组疼痛恶化的时间
与基线相比,两个治疗组所有随访患者的BPI-SF最严重疼痛、单项最严重骨痛和FACT-P TOI最小二乘平均变化均保持稳定。奥拉帕利组和安慰剂组的FACT-P TOI的校正平均改变分别是-0.10和-1.20(差 1.30,p=0.52)。两组疼痛恶化的时间相似(BPI-SF最严重疼痛HR 0.90, p=0.30;最严重骨痛HR 0.85,p=0.18)。从基线到第48周,两组EQ-5D-5L疼痛和不适方面的改善率相似。
综上,在该探索性分析中,奥拉帕利与阿比特龙联合使用时,对前列腺癌患者的疼痛和HRQOL没有显著影响。总而言之,该联合方案可显著延长前列腺癌患者的影像学无进展生存期,且不会影响期生活质量。
原始出处:
Fred Saad, et al. Patient-reported outcomes with olaparib plus abiraterone versus placebo plus abiraterone for metastatic castration-resistant prostate cancer: a randomised, double-blind, phase 2 trial. Lancet Oncol. September 02, 2022. https://doi.org/10.1016/S1470-2045(22)00498-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
0
#抗性#
60
#Oncol#
41
期待PFS及OS的结果,这些才有真正的说服力。感觉这个实验设计的有问题,没有区分队列,至少应该检测BRCA或者HRD,然后进行队列分组,我觉得这样设计可能更合理些。
45
#去势抵抗性前列腺癌#
0
#转移性#
41
谢谢分享
37