Neurology:来自丹麦和瑞典的双国家队列研究:丧子之痛增加父母卒中发生风险,需更多社会支持与关注!
2022-02-19 Naomi MedSci原创
近日,有研究人员调查了失去子女的父母是否有更高的卒中风险,并分析造成相关风险差异的因素。研究发现,孩子去世与父母发生卒中的风险略有增加有关。这提示需要家庭成员和医疗保健专业人员提供更好的支持和关注。
儿童死亡是一个极端的生活事件,对家庭有潜在的长期健康影响。越来越多的证据表明,经历过子女死亡的父母比未有相关经历的父母有更高的发病率和死亡率,包括心肌梗死、冠状动脉疾病、心室颤动、心力衰竭和心源性猝死。最近的一项系统综述表明,近亲的死亡与卒中风险的增加有关,然而,审查中包括研究中的大多数都集中在配偶的丧亲之痛上。到目前为止,只有一项研究调查了18岁以下儿童的死亡与卒中之间的关系,这可能是因为父母在随访结束时还太小不能经历卒中。
近日,在一项以人群为基础的队列研究中,在长达39年的随访追踪中,有研究人员调查了失去子女的父母是否有更高的卒中风险,如果有的话,风险是否因孩子的死亡特征、死亡时间、家庭的社会人口因素或卒中的亚型而有所不同。
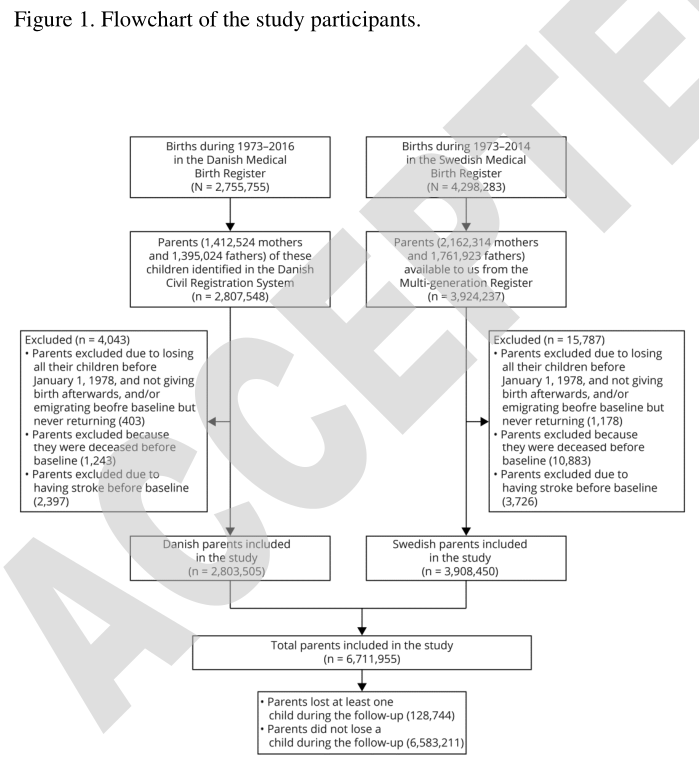
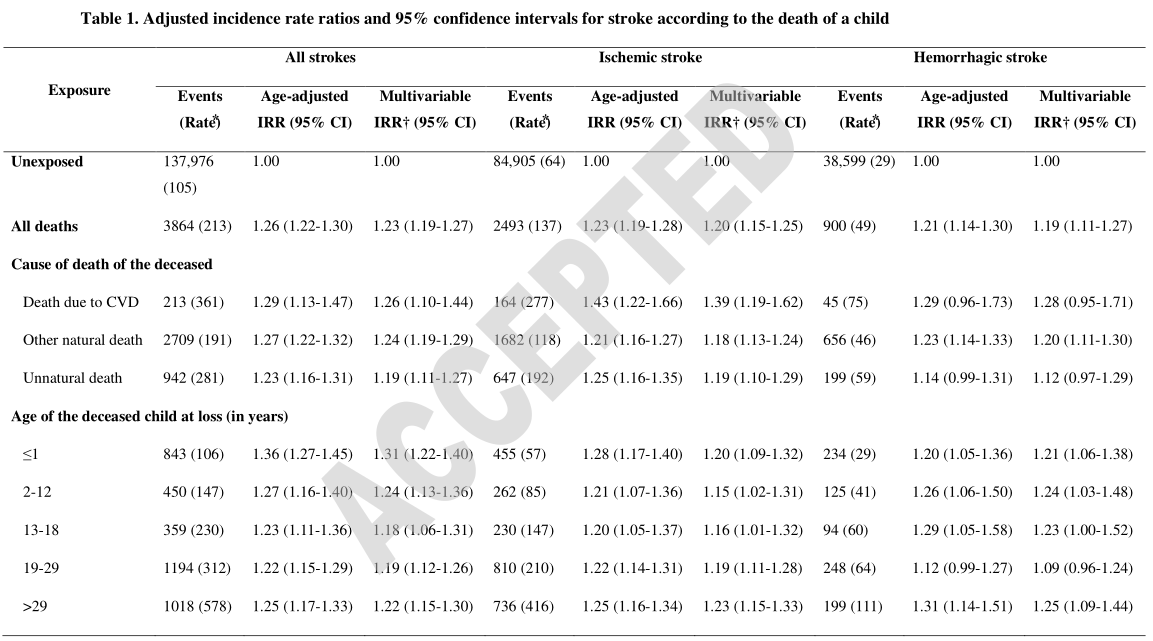
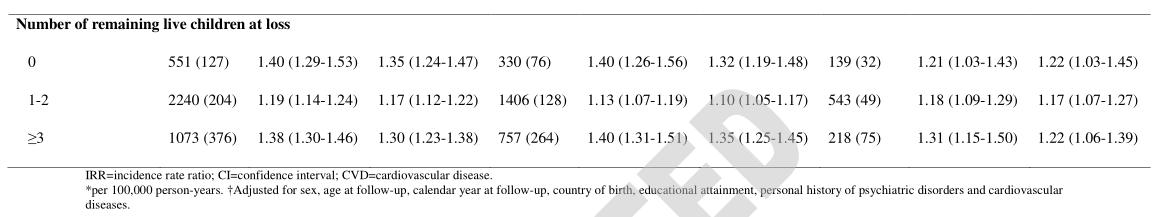
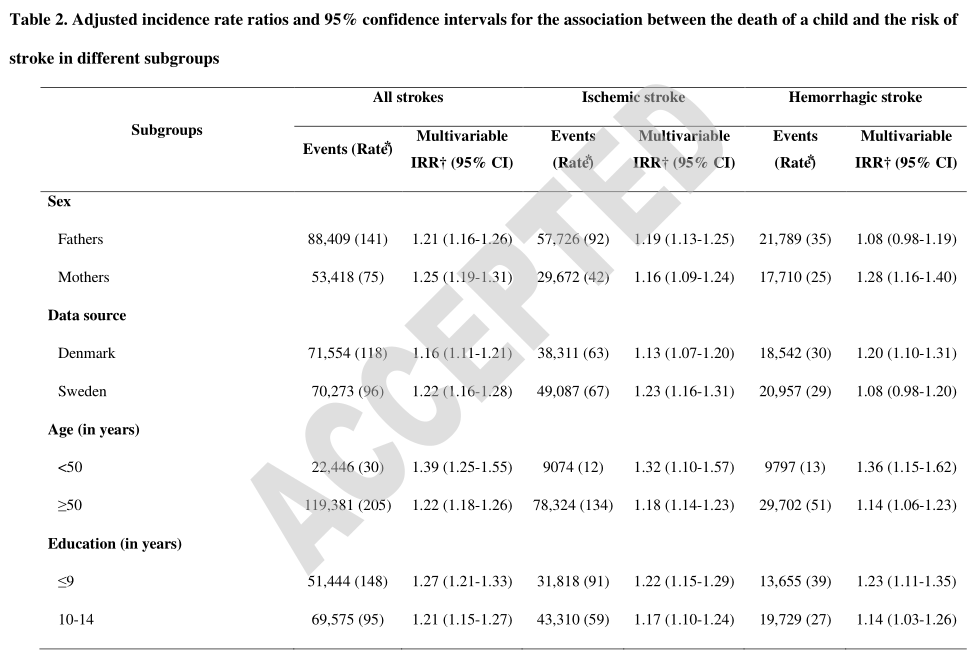
研究人员进行了一项基于人口的队列研究,研究对象包括在1973-2016年或1973-2014年期间出生并分别记录在丹麦和瑞典医学出生登记册中的子女的父母。通过几个人口登记册之间的联系获得了有关儿童死亡、父母卒中以及社会经济和健康相关特征的信息。使用泊松回归来研究儿童死亡和卒中风险之间的联系。
- 在6,711,955名研究参与者中,有128,744人(1.9%)在随访期间死亡,141,840人(2.1%)卒中。
- 失去双亲者卒中危险性增加,相应的发病率比(95% 置信区间)为1.23(1.191.27)。在所有分析的儿童死亡原因(心血管疾病、其他自然死亡和非自然死亡)中,这种联系都存在,且并没有根据死亡子女的年龄而差异,但如果父母在丧子时没有子女或≥3个活着的子女,则强于1-2个活着的子女。
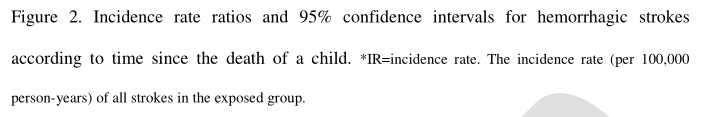
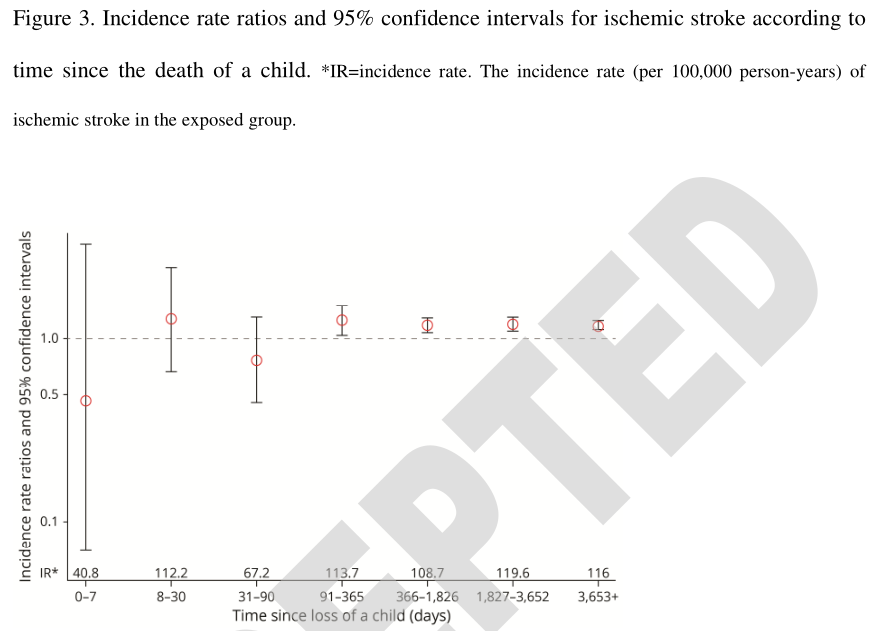
- 缺血性和出血性卒中也有类似的联系。父母出血性卒中的风险在儿童死亡后立即达到最高值,之后降低。相反,在缺血性卒中的病例中,随着时间的推移并没有明显的模式。
孩子去世与父母发生卒中的风险略有增加有关。在非自然死亡案例中观察到的联系的发现提示了丧亲相关的压力可能促进卒中发展的解释。虽然儿童的死亡往往无法避免,但了解其与健康有关的后果可能会突出表明,需要家庭成员和医疗保健专业人员提供更好的支持和关注。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#Neurol#
25
#国家队#
32
认真学习了
52
好!
42
#社会#
30