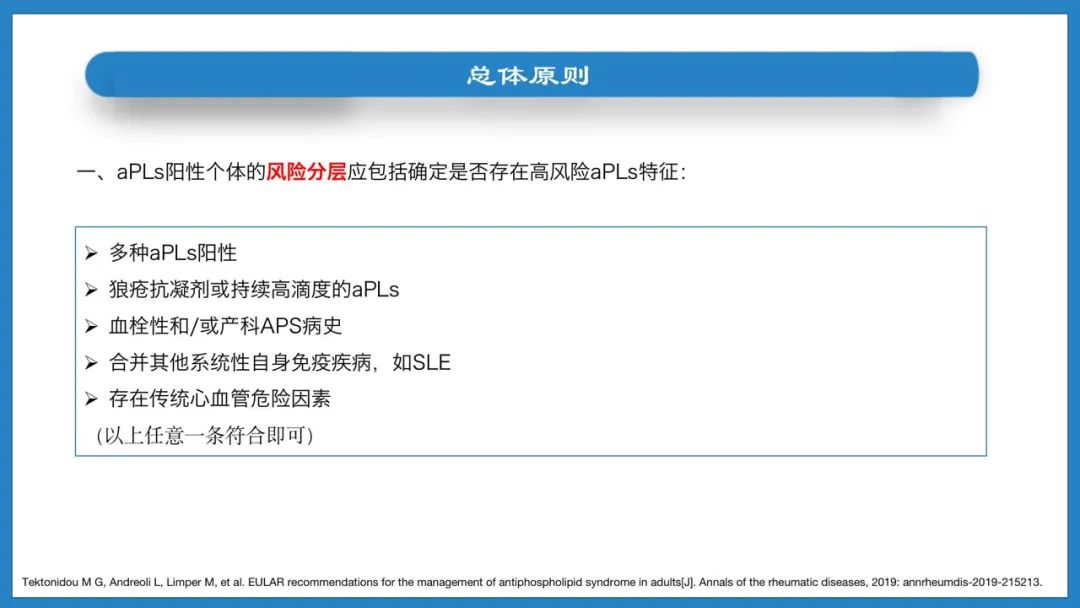
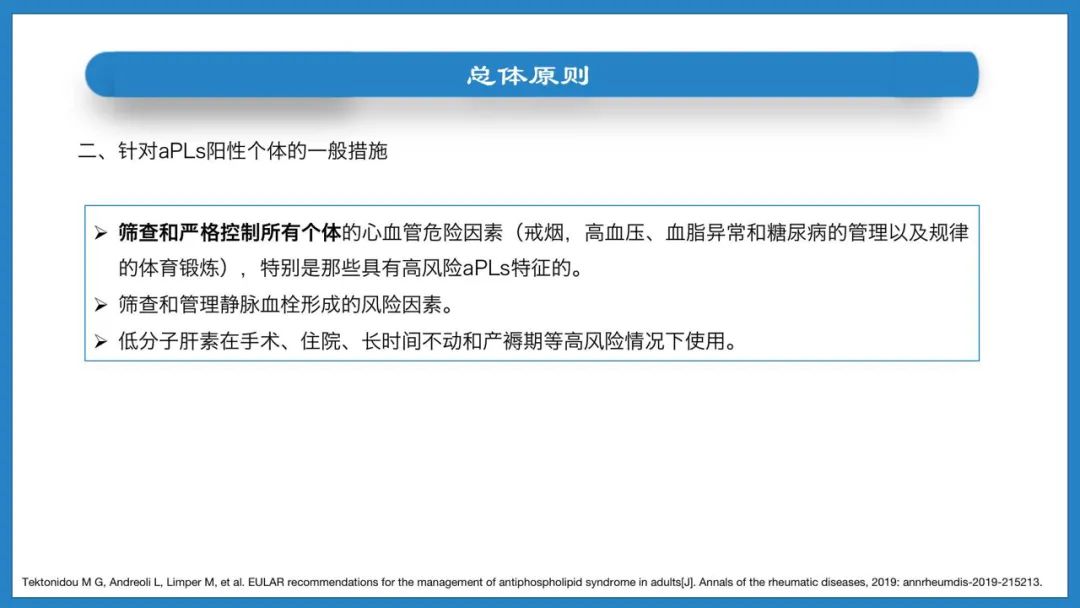
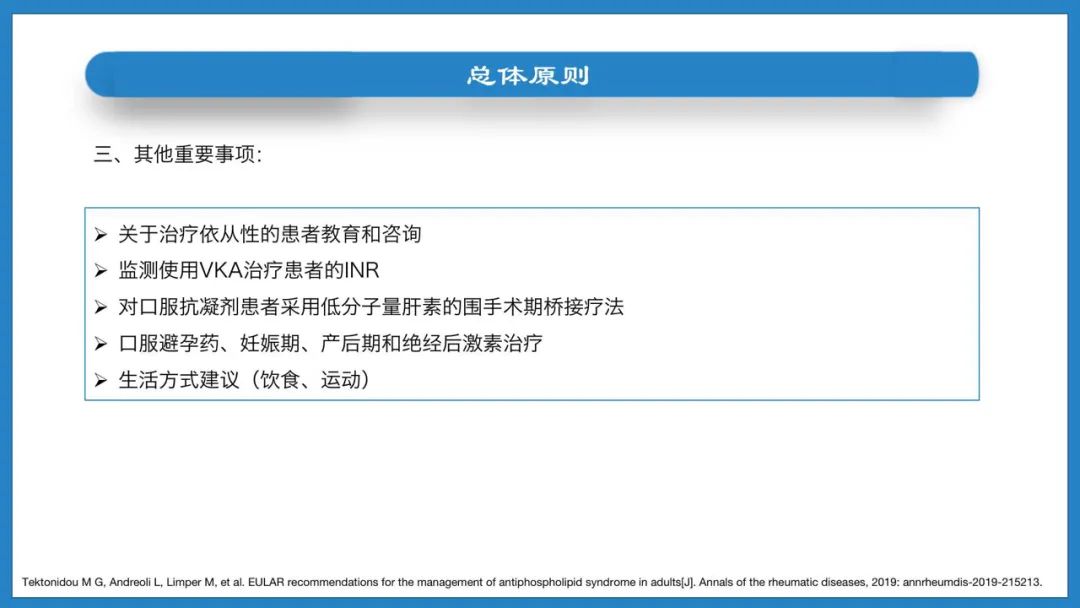
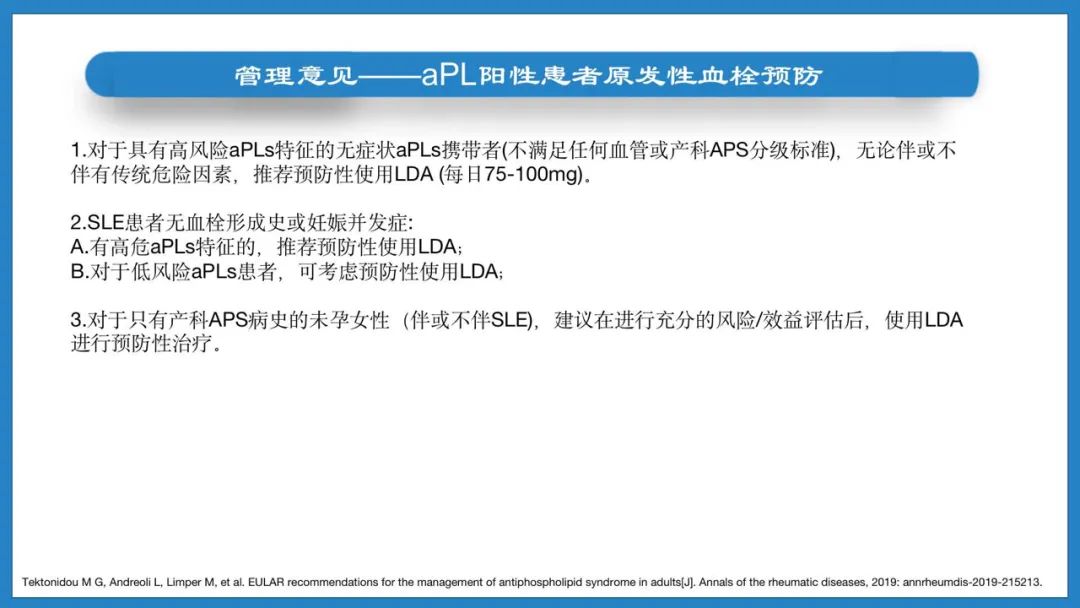
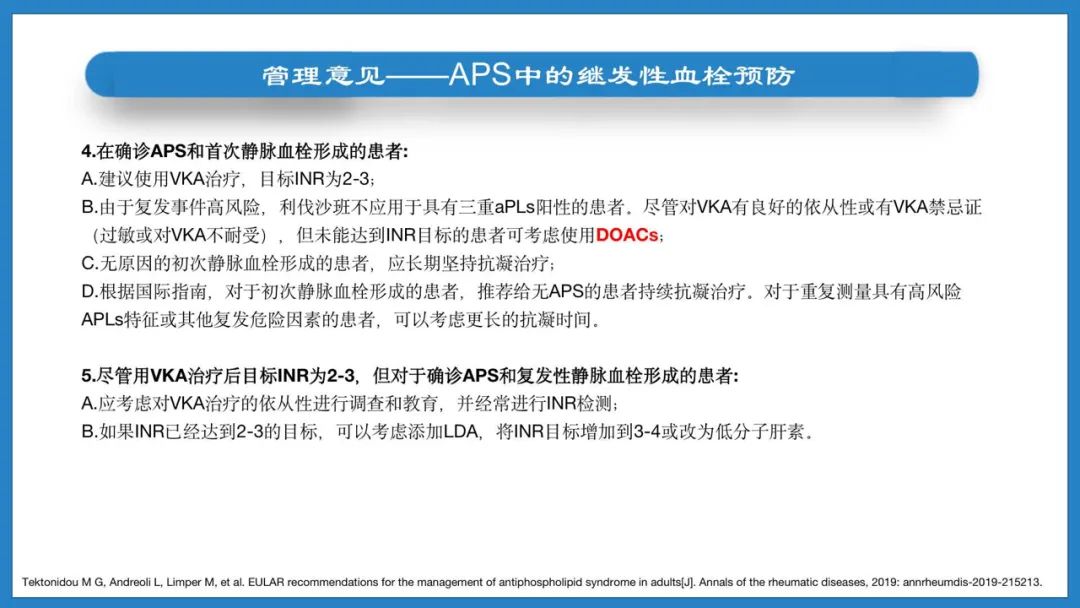
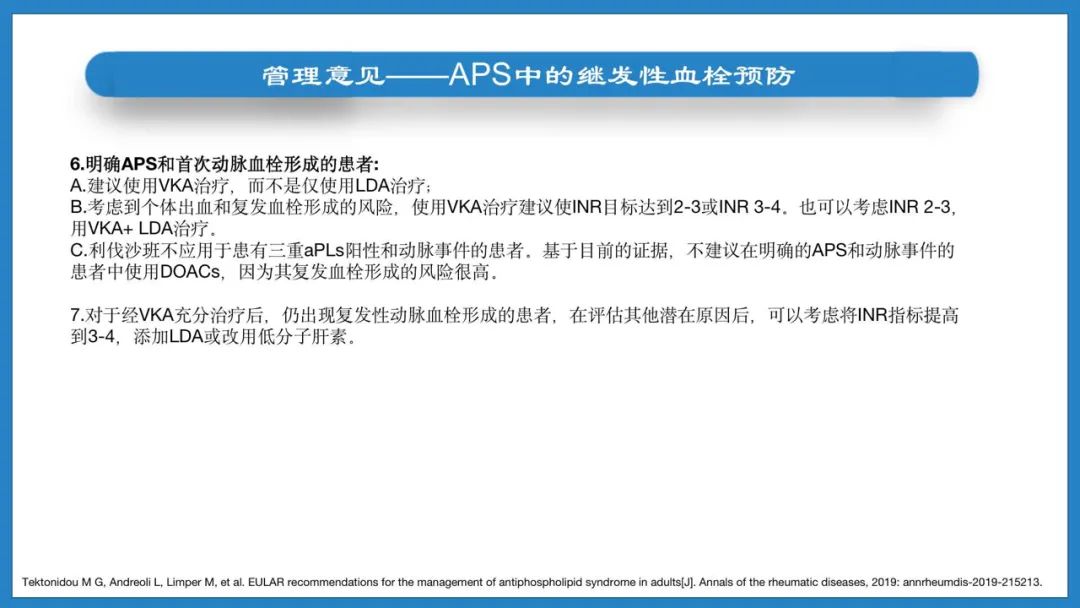
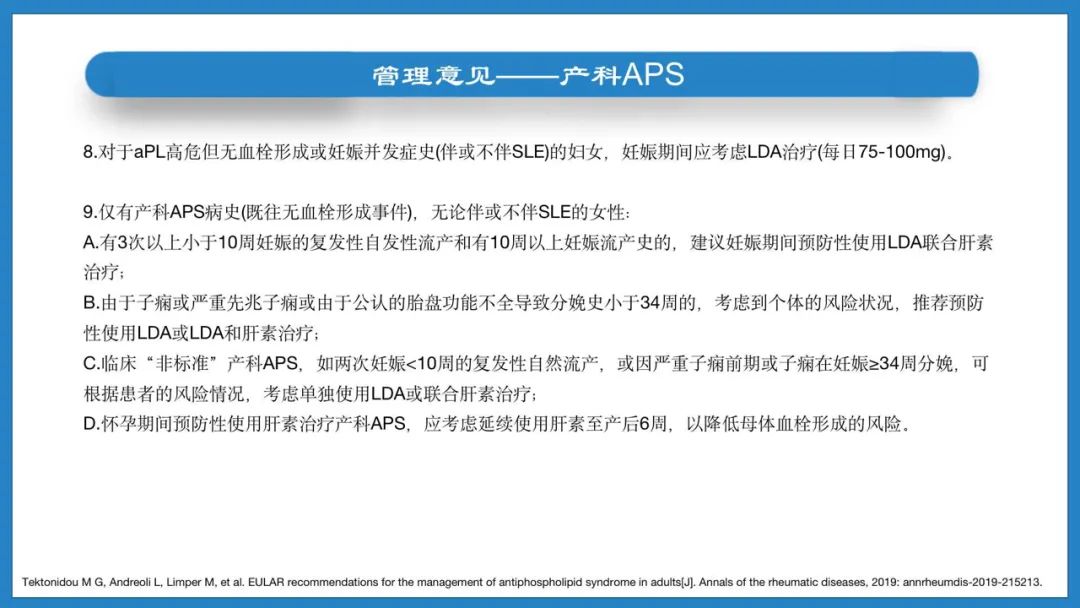
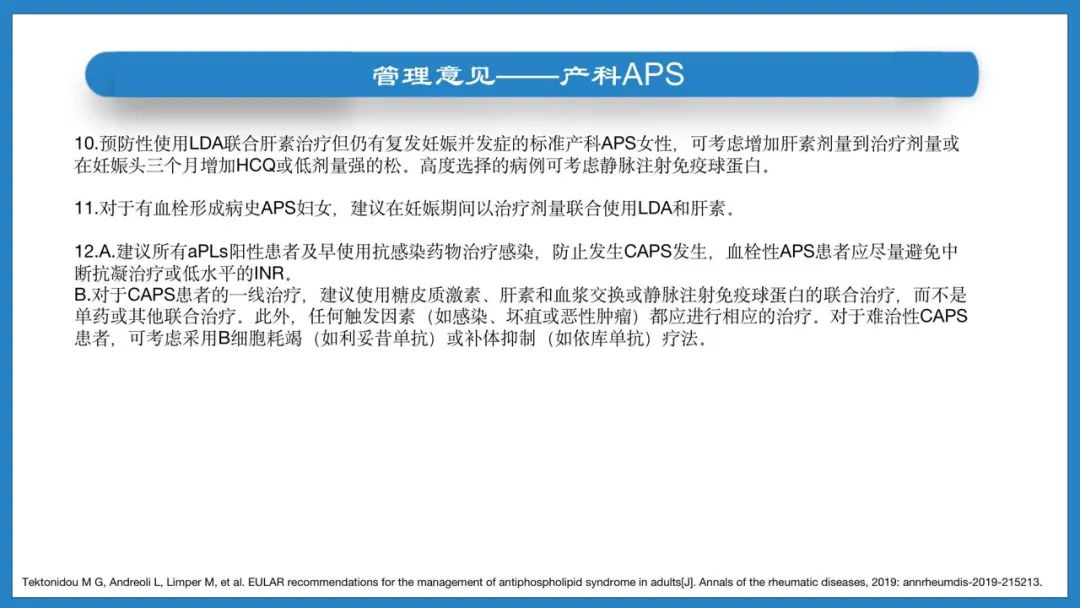
2019年EULAR建议:成人抗磷脂综合征的管理
2021-11-05 张磊 岭南风湿
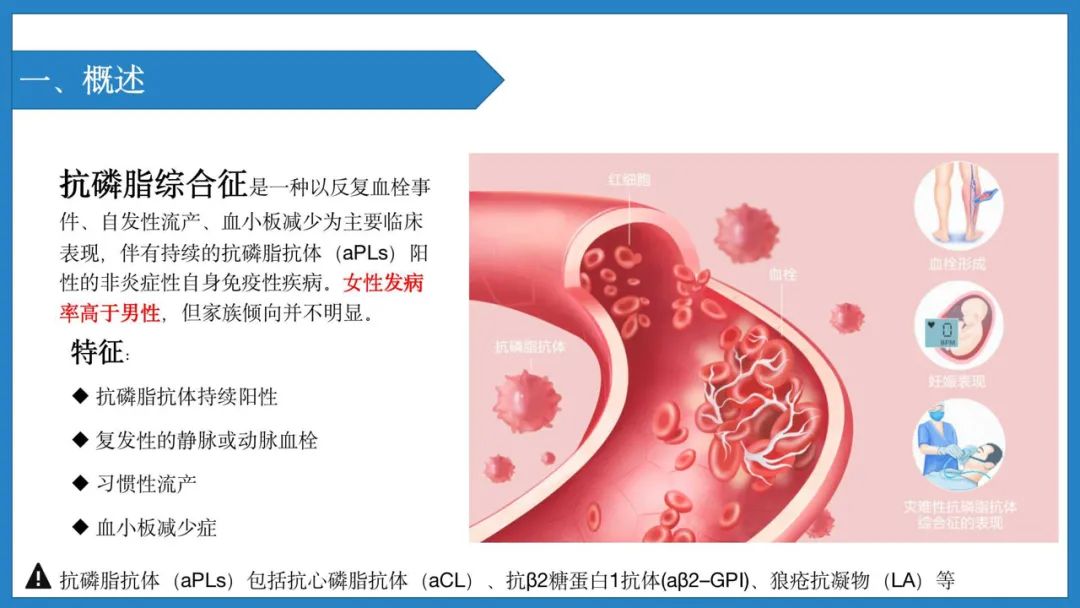
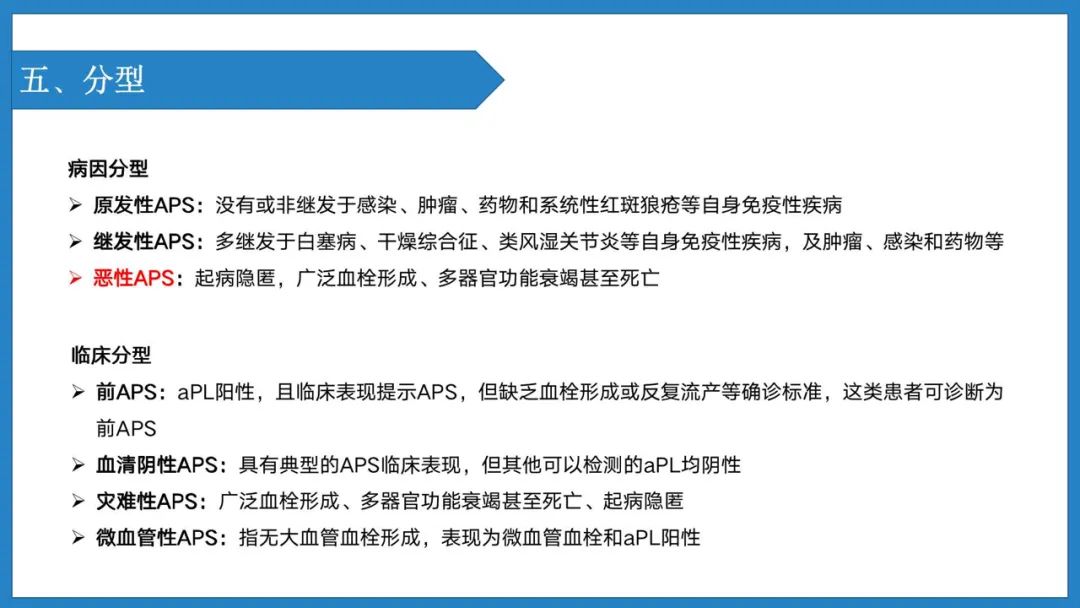
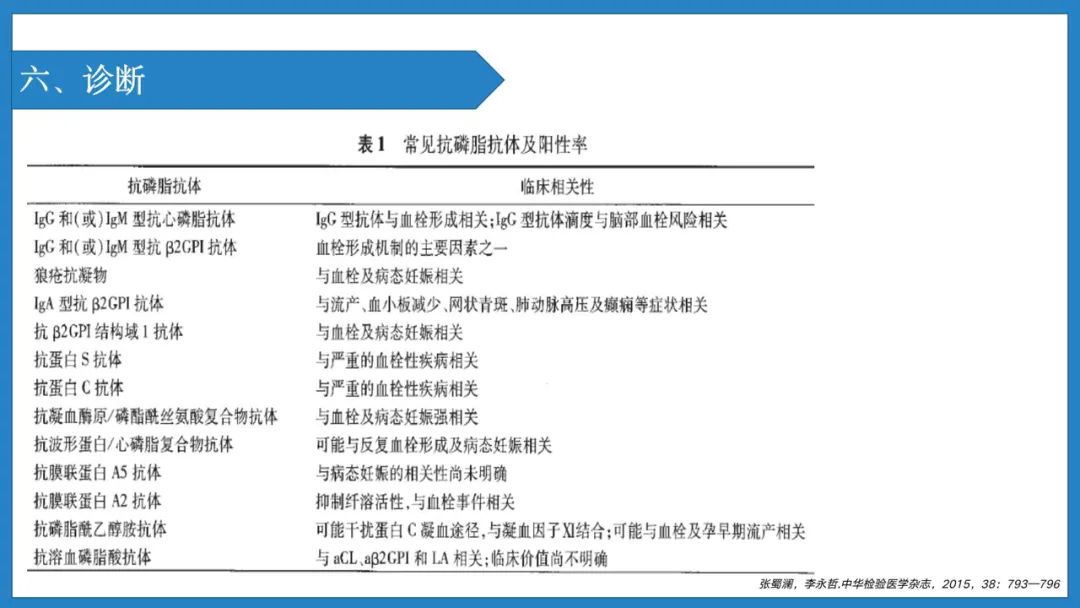
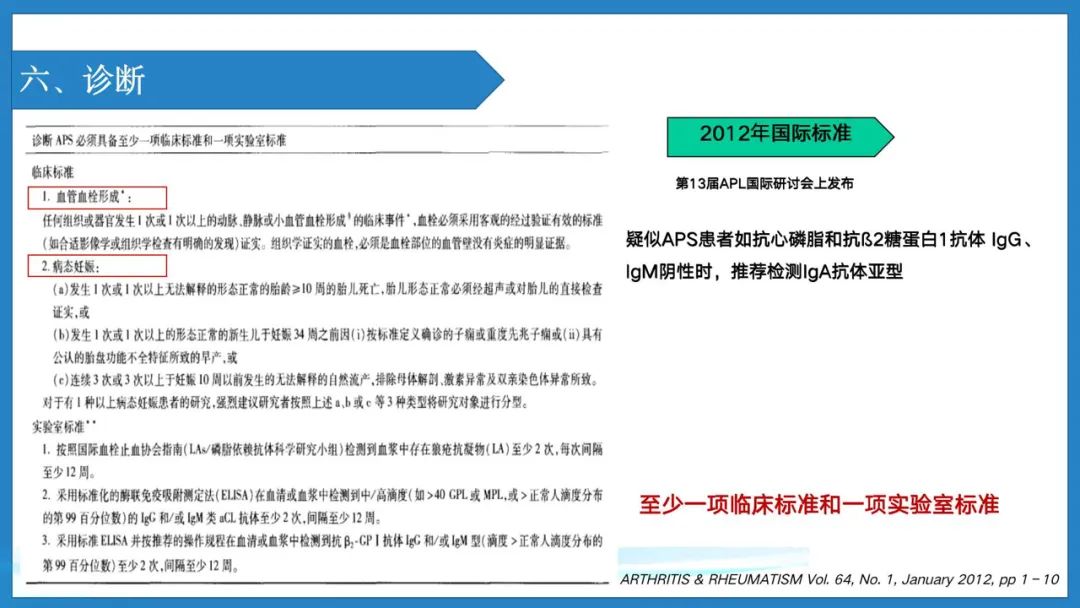
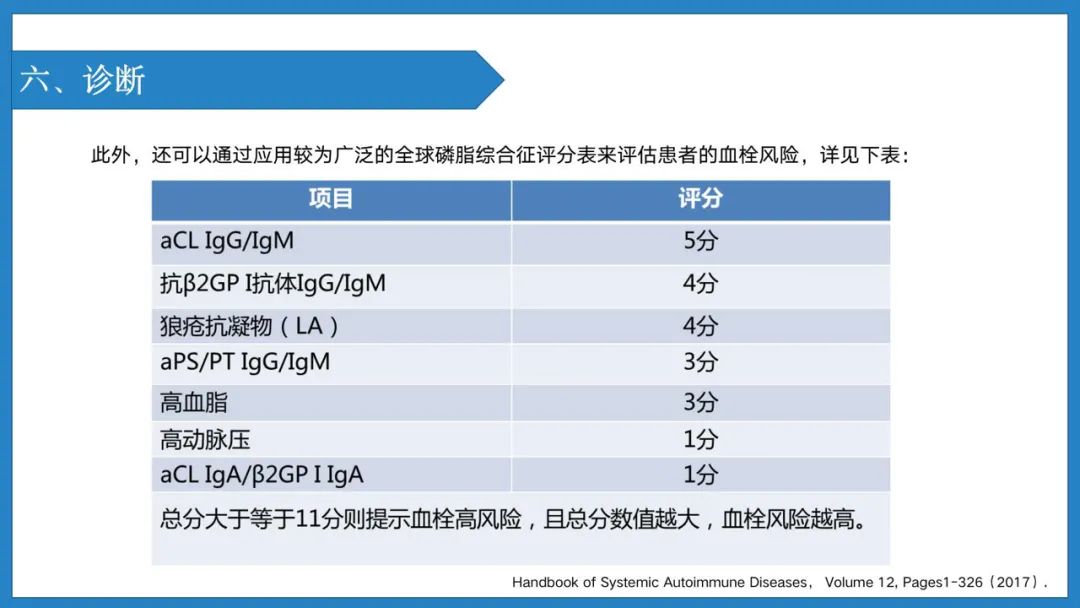
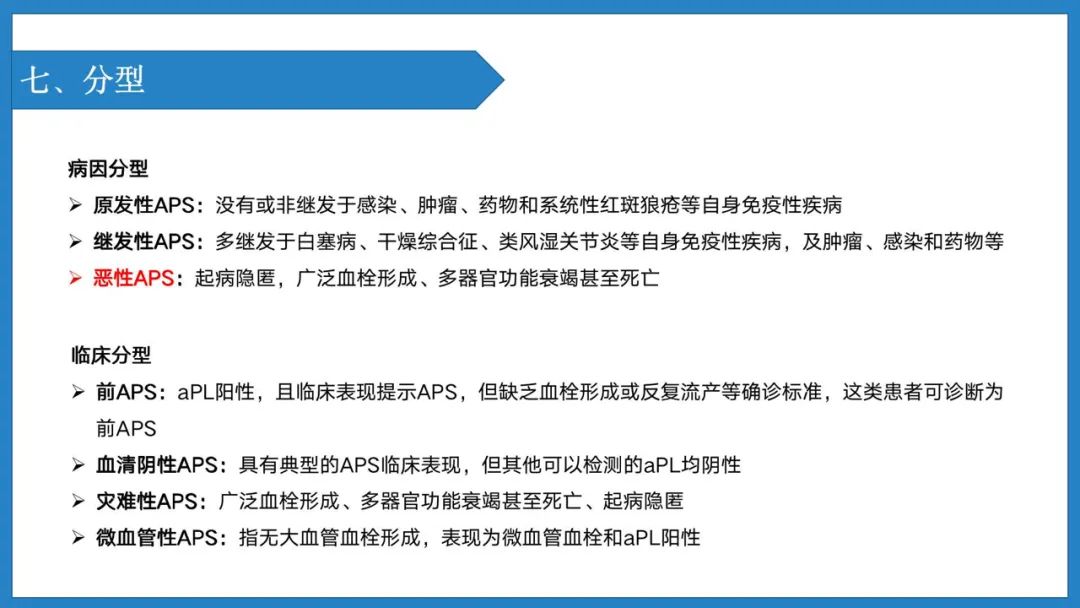
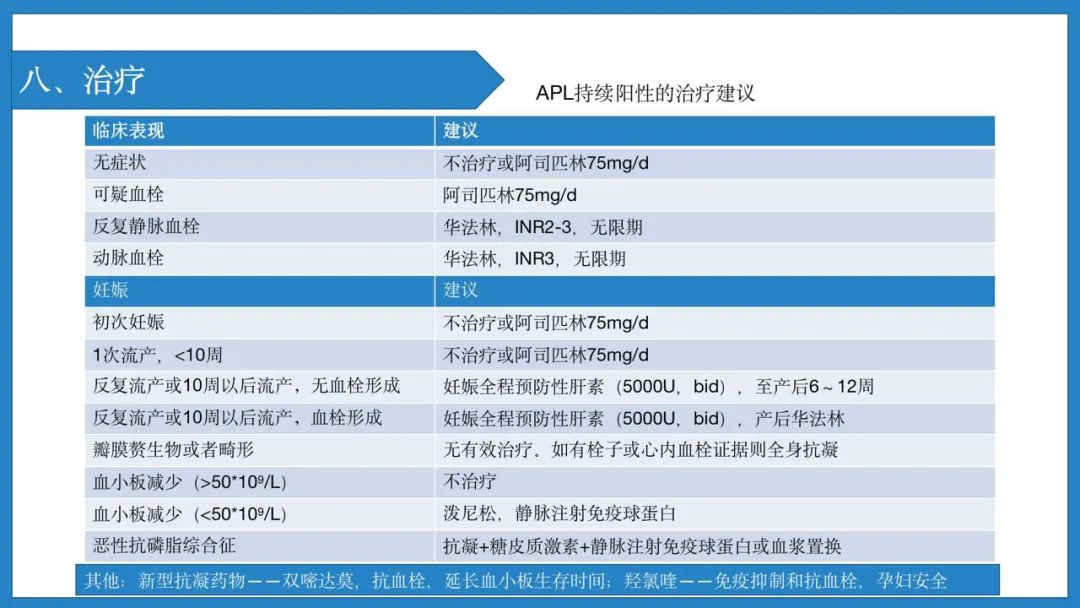
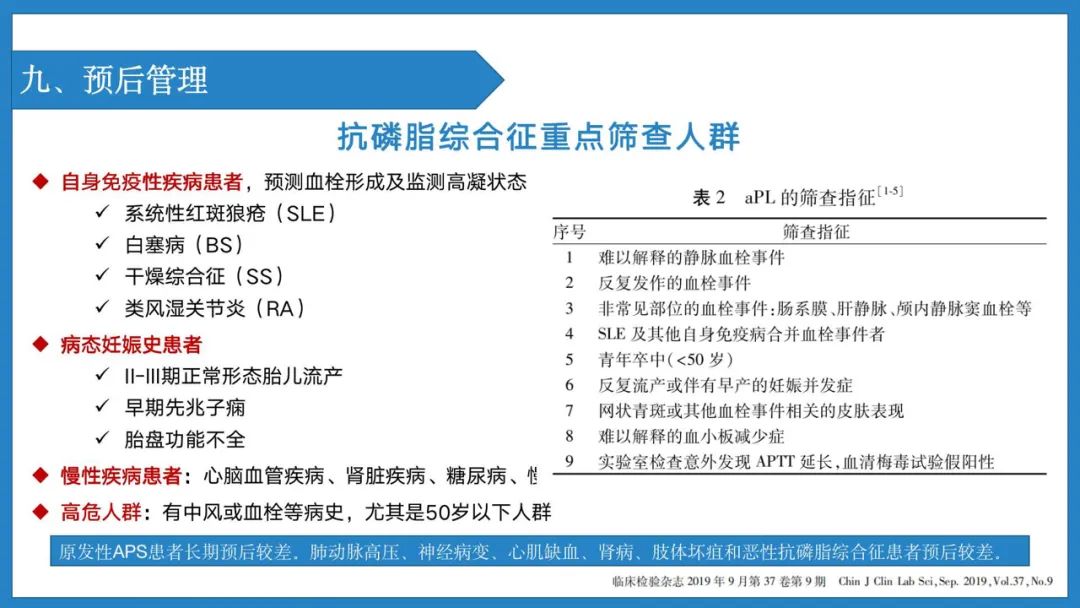
抗磷脂综合征是以抗磷脂抗体持续阳性、复发性的静脉或动脉血栓、习惯性流产和血小板减少症为特征的非炎性自身免疫性疾病。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了,非常感谢
49
学习
34
感谢分享,大牛
35
感谢分享
42
#综合征#
33
#EULAR#
38
谢谢分享
51
#学习#、很好的`冂内容,学]习了。
40
谢谢分享
36