JCEM:绝经后妇女的脆性骨折预测
2022-02-19 MedSci原创 MedSci原创
该研究推导出的三个模型以精确预测骨折,特别是对于MOF和躯干骨折。这些模型基于数量有限的CRF,研究人员构建了可用于临床实践的列线图。
骨质疏松症是一个严重的公共卫生问题,全世界有超过2亿人发生脆性骨折的风险增加,导致过早死亡或由于急性疼痛、长期疾病和残疾而导致生活质量下降。这也造成了沉重的社会经济负担。药物治疗可将骨折发生率降低30%至60%,并将骨折后死亡率降低10%。然而,尽管现有药物治疗有效,但只有20%至30%的骨折高风险女性得到了有效治疗。个体化骨折风险评估可能有助于选择需要药物治疗的骨质疏松症患者。FRAX和Garvan骨折风险计算器是最常用的工具,尽管它们的外部验证显示其风险预测能力存在显著差异。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员使用来自FRISBEE研究的数据,纳入了3560名60-85岁的绝经后女性。研究人员旨在使用经过验证的临床风险因素(CRF)构建5年骨折风险预测模型。
研究人员开发了三种竞争风险分析模型来预测主要骨质疏松性骨折(MOF)、所有骨折和躯干骨折(股骨颈、肩部、临床脊柱、骨盆、肋骨、肩胛骨、锁骨、胸骨)。
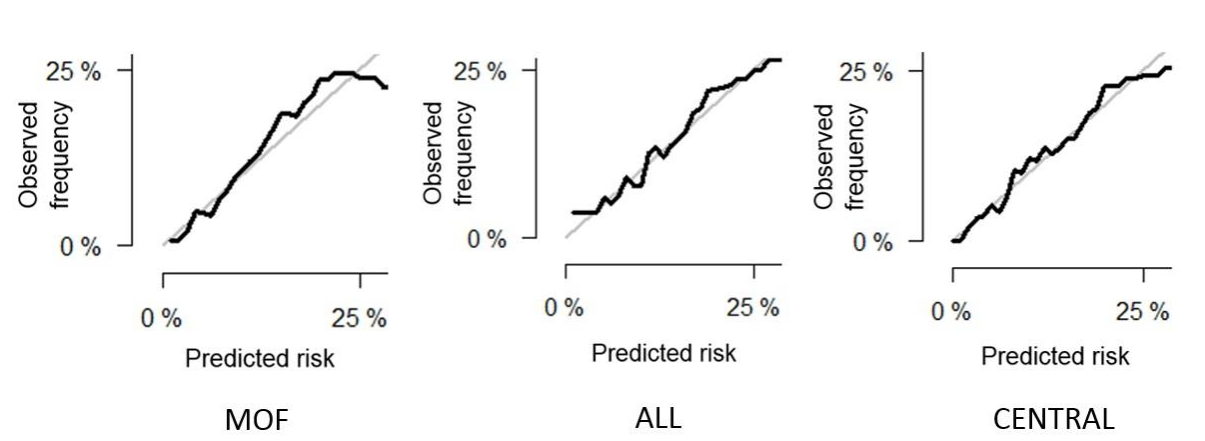
年龄、骨折史和髋关节或脊柱骨密度是三个模型的共同预测因素。过量饮酒和合并症是MOF的特定额外CRF、所有骨折的跌倒史和躯干骨折的类风湿关节炎。该模型预测5年的骨折概率具有可接受的准确性(Brier评分≤0.1),并且在通过bootstrap进行内部验证时具有良好的辨别能力(MOF的受试者操作曲线下面积为0.73,躯干骨折为0.72)。为不同的骨折部位构建了三个简单的列线图,整合了显著的CRF和死亡风险。
总之,该研究推导出的三个模型以精确预测骨折,特别是对于MOF和躯干骨折。这些模型基于数量有限的CRF,研究人员构建了可用于临床实践的列线图。
原始出处:
Felicia Baleanu.et al.Fragility fractures in postmenopausal women: development of 5-year prediction models 2 using the FRISBEE study.JCEM.2022.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgac092/6530319
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCE#
33
#JCEM#
29
#绝经#
40
#绝经后妇女#
42
#脆性骨折#
61
#绝经后#
34
看看,现在要注意啦
59