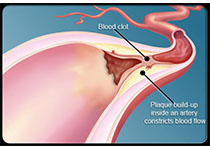
Stroke:DVT/PE:DOACs的优越性再添一项 ICH显著降低
2018-08-08 王淳 环球医学
静脉血栓栓塞症(VTE),包括深静脉血栓形成(DVT)、肺栓塞(PE)等,严重影响患者生存率。抗凝药是重要的治疗选择。长期以来,华法林一直是标准的抗凝治疗药物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DVT/PE#
32
#PE#
23
#DVT#
42
好好学习天天向上
84
#ACS#
25
#ICH#
34
#DOACs#
40
作者从极其专业的角度论述了大结节角的测量方法,使我们对影像学的专业诊断知识有了进一步的了解,多谢分享!
66
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
51