N Engl J Med:肿瘤突变负荷能为纳武单抗一线治疗晚期NSCLC争取一席之地吗
2017-06-29 佚名 肿瘤资讯
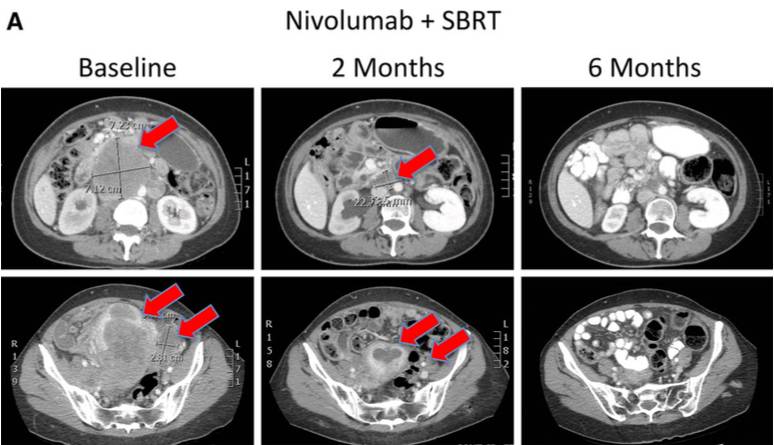
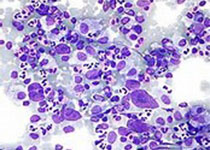
晚期NSCLC一线含铂化疗的中位PFS为4~6个月,OS为10~13个月。针对一线含铂方案进展晚期NSCLC,2项3期研究证明较标准二线多西他赛联合纳武单抗显着延长OS。尽管肺腺癌中PD-L1表达增加疗效提高,但总体上纳武单抗疗效与PD-L1表达相关性差。1期checkmate012研究,初治晚期NSCLC20例,其中10例PD-L1表达≥5%,ORR 50%,24周PFS率70%,中位PFS 1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Eng#
35
#肿瘤突变#
0
#Engl#
31
#晚期NSCLC#
34
#肿瘤突变负荷#
30
#Med#
23
学习了,谢谢分享
45
PD-L1应该大于25%?
60