JAHA:术前右心室游离壁纵向应变可作为严重三尖瓣关闭不全术后的预后指标
2021-04-18 MedSci原创 MedSci原创
术前RVFWSL作为RV功能障碍的指标是接受重度功能性TR手术患者的独立预后指标。因此,术前RVFWSL可以帮助判断严重功能性TR患者的最佳手术时机。
在发生不可逆的右心室(RV)功能障碍之前,应对严重的三尖瓣关闭不全(TR)进行干预。但是,当前的指南并未提供与RV收缩功能相关的标准来指导最佳手术时机。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员纳入了115例连续就诊的患者(年龄为62±10岁;男性占23.5%;62.6%[n=72]的患者先前接受过左侧瓣膜手术),他们在两个三级中心接受了重度功能性TR手术。

研究人员收集了患者术前的临床和超声心动图参数,包括RV游离壁纵向应变(RVFWSL)。该研究的主要终点是心脏死亡和手术后5年归因于心血管原因的计划外再入院的综合结局。
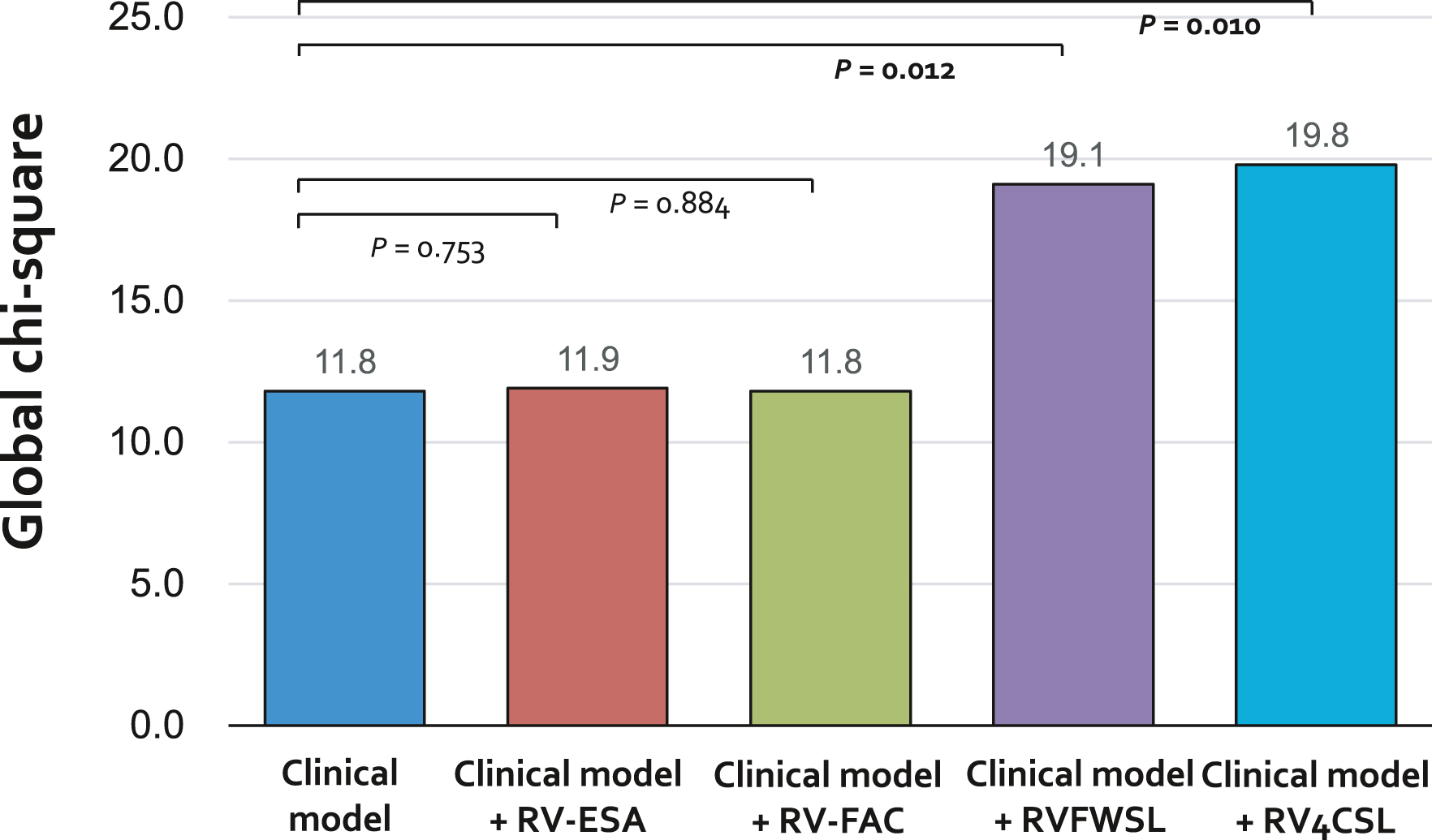
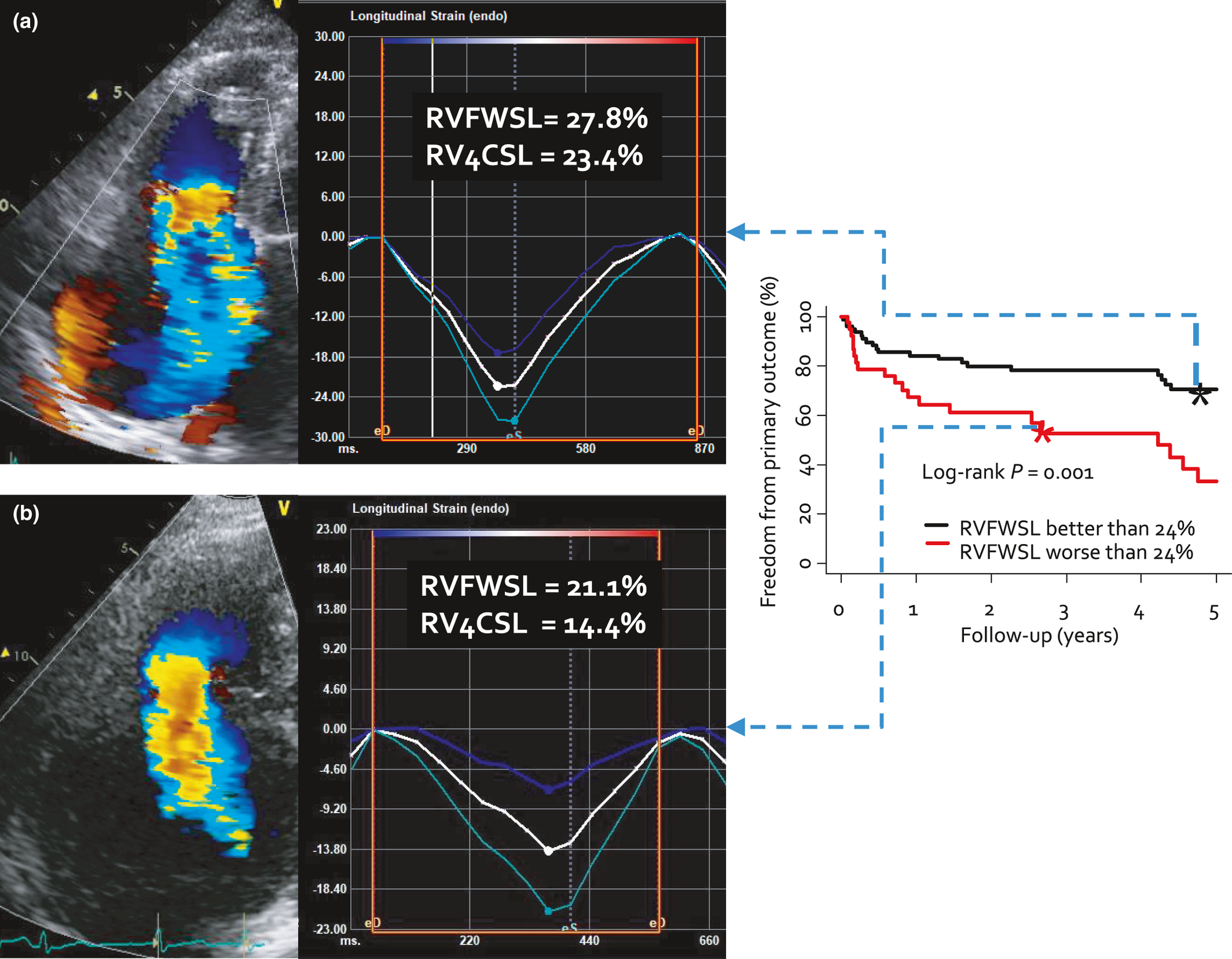
在333人次每年的随访期间,有40例患者(34.8%)出现了主要终点。由于心血管原因,有11例患者发生心源性死亡和34例患者出现计划外再入院治疗,其中5例两种情况均经历过。术前绝对RVFWSL<24%与主要终点相关(风险比为2.30;95%CI为1.22-4.36;P=0.011),与临床风险因素无关,包括欧洲心脏手术风险评估系统II和血红蛋白水平。同时,RV收缩功能的其他常规超声心动图指标并不显著。将RVFWSL绝对值<24%添加到临床模型增加了其对主要终点的预测价值。
由此可见,术前RVFWSL作为RV功能障碍的指标是接受重度功能性TR手术患者的独立预后指标。因此,术前RVFWSL可以帮助判断严重功能性TR患者的最佳手术时机。
原始出处:
Minkwan Kim.et al.Preoperative Right Ventricular Free‐Wall Longitudinal Strain as a Prognosticator in Isolated Surgery for Severe Functional Tricuspid Regurgitation.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.019856
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#AHA#
37
#预后指标#
43
#右心室#
51
#三尖瓣#
36
学习了
51