JGH: 抗血栓药物对食管内镜下切除延迟出血的影响
2022-09-15 xuyihan MedSci原创
ESD是一种英文缩写,在医学上主要指的是内镜黏膜下剥离术。一般是用于治疗间质瘤、息肉等胃肠道良性或者低度恶性肿瘤的一种常用方法,可以代替传统的外科手术。
内镜黏膜下剥离术 (ESD) 是消化道肿瘤整块切除的可靠方法;它具有高治愈性、微创性,目前已成为无转移的胃肠道肿瘤的标准治疗方法。内镜下黏膜切除术 (EMR) 已成为食管癌小病变的首选治疗方法。延迟出血是ESD和EMR最常见的不良事件之一,据报道,胃中的发生率为5.3-5.7%,结肠中的发生率为 1.4-8.5%。然而,食管ESD后出血很少见,据报道发生率仅为0.4%。近年来,随着缺血性疾病发病率高的成年人群的老龄化,服用抗血栓药物的患者数量不断增加。一份报告表明,接受内窥镜检查的患者中有15.5%正在服用抗血栓药物。阿司匹林、噻吩并吡啶、直接口服抗凝剂 (DOAC) 和华法林被认为是具有出血风险的抗血栓药物。然而,停用这些药物会增加血栓栓塞事件的风险。日本胃肠病学内窥镜学会 (JGES) 指南将胃、结肠和食管内镜下切除术 (ER) 归类为具有高出血风险的手术。因此,尚不清楚食管后ER出血的风险是否会随着这些药物的使用而增加。因此,本研究旨在调查使用抗血栓药物(即阿司匹林、噻吩并吡啶、DOAC和华法林)和中断后其对食管ER术后出血的影响。

本项研究共招募了957名接受内镜切除术的患者(总共有1202例食管肿瘤),并根据抗血栓药物的使用情况将其分类为未使用组、阿司匹林组、噻吩并吡啶组、DOAC组和华法林组。使用抗血小板药物(即阿司匹林和噻吩并吡啶)的患者根据内镜切除前继续或停止使用进一步细分。最后比较这些组之间的出血率的差异,以评估使用抗血栓药物和中断抗血小板治疗对食管内镜切除术后出血的影响。

研究结果显示:未使用抗血栓药物组内镜切除术后出血率为 0.3%(95% CI,0.1-1),继续服用阿司匹林组为 4.5%(95% CI,0.1-23),阿司匹林停药组为2.9%(95% CI,0.1-15),阿司匹林联合噻吩并吡啶组为0%(95% CI,0-78),噻吩并吡啶停药组为0%(95% CI,0-26), DOAC组为13%(95% CI,1.6-38),华法林组为 0%(95% CI,0-45)。DOAC组内镜下切除术后出血率明显高于未使用抗栓药物组(P=0.003)。然而其他组之间的内镜切除术后出血率没有差异。
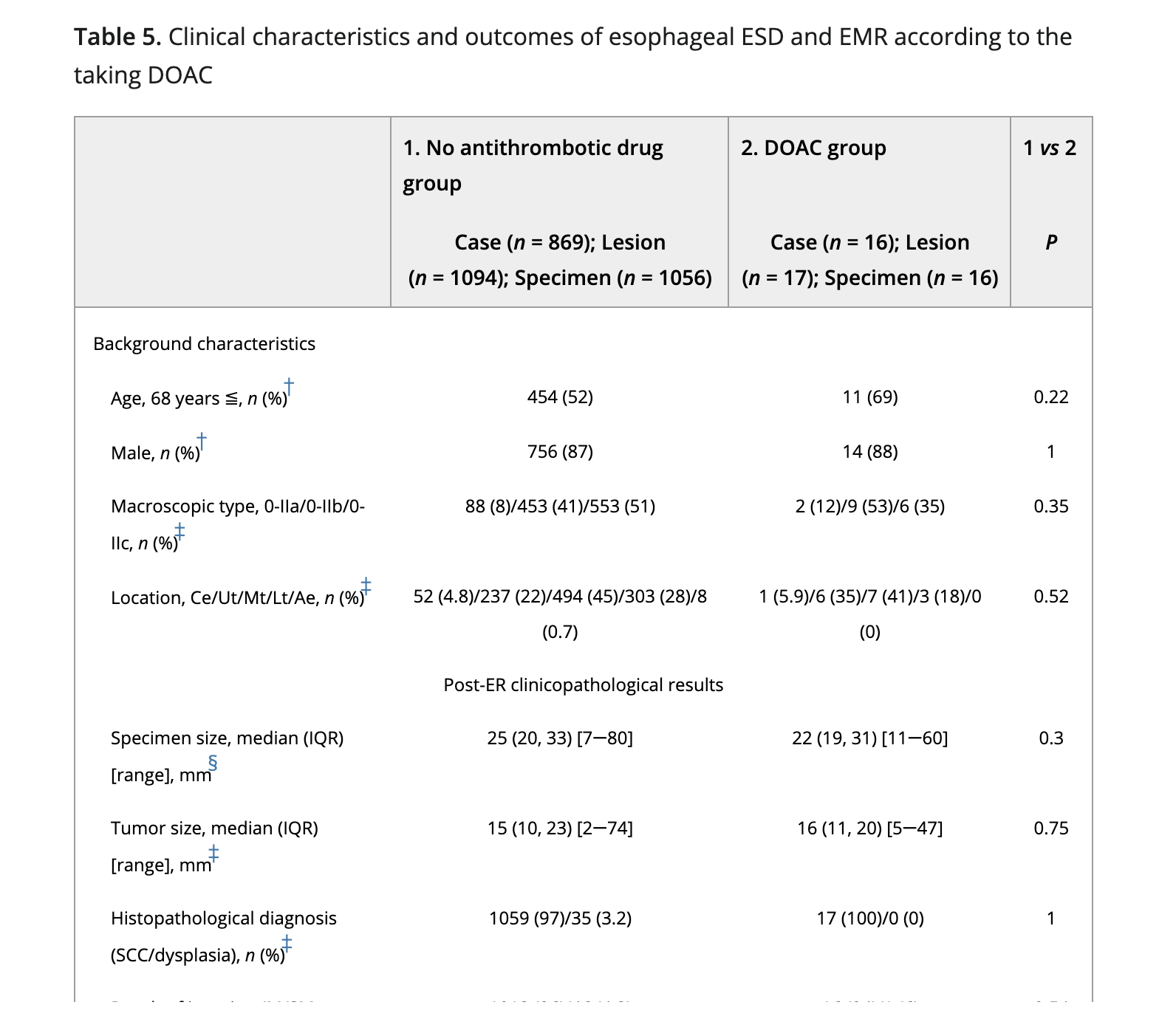
本项研究结果表明食管内镜切除术不需要停用阿司匹林,但是必须要关注使用DOAC药物的这部分病人,因为他们的术后出血率要高于其他患者。
原始出处:
Yoshimasa Horie. et al. The effect of antithrombotic drug use on delayed bleeding with esophageal endoscopic resection. Journal of Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抗血栓药物#
49
#内镜下切除#
52
#抗血栓药#
40
#内镜#
67
#食管#
47
#抗血栓#
33