European radiology:肺动脉高压(PAH)、肺静脉闭塞性疾病及肺毛细血管血管瘤并(PVOD/PCH)的双能量CT肺灌注特征
2022-07-13 shaosai MedSci原创
在第六届世界肺动脉高压(PH)研讨会上将PAH重新分类,成人PAH类别包括特发性PAH、遗传性PAH、药物和毒素引起的PAH、与不同疾病相关的PAH、对钙通道阻滞剂有长期反应的PAH。
 肺动脉高压(PAH)是肺动脉高压症的原因一直,其特点是肺小动脉的增生性重塑和纤维化。在第六届世界肺动脉高压(PH)研讨会上将PAH重新分类,成人PAH类别包括特发性PAH、遗传性PAH、药物和毒素引起的PAH、与不同疾病(结缔组织病、HIV感染、门静脉高压、先天性心脏病、血吸虫病)相关的PAH、对钙通道阻滞剂有长期反应的PAH以及有静脉/毛细血管受累明显特征的PAH。 后者也被称为肺静脉闭塞性疾病和/或肺毛细血管瘤病(PVOD/PCH),被认为是PH的一个难以诊断的亚组。
肺动脉高压(PAH)是肺动脉高压症的原因一直,其特点是肺小动脉的增生性重塑和纤维化。在第六届世界肺动脉高压(PH)研讨会上将PAH重新分类,成人PAH类别包括特发性PAH、遗传性PAH、药物和毒素引起的PAH、与不同疾病(结缔组织病、HIV感染、门静脉高压、先天性心脏病、血吸虫病)相关的PAH、对钙通道阻滞剂有长期反应的PAH以及有静脉/毛细血管受累明显特征的PAH。 后者也被称为肺静脉闭塞性疾病和/或肺毛细血管瘤病(PVOD/PCH),被认为是PH的一个难以诊断的亚组。
在对PH的潜在原因进行分层时,目前的指南建议进行V/Q肺部闪烁术来寻找CTEPH。CTEPH的识别是基于对无灌注但通气功能保留的肺段或亚段的识别。自双能CT(DECT)问世以来,人们对DECT肺灌注图像上的肺部微循环的分析产生了极大的兴趣。虽然这些图像不是严格意义上的灌注图像,但可作为肺部灌注评估的适当替代标记物。在PH方面,DECT肺灌注主要在CTEPH中进行了研究,显示出与闪烁术检测灌注缺陷的良好一致性以及与PH严重程度的血流动力学估计的良好相关性。据我们所知,目前还没有具体的研究来评估DECT肺灌注提供PAH和PVOD/PCH之间的明显特征。
近日,发表在European radiology杂志的一项研究比较了DECT检查中特发性或遗传性PAH和PVOD/PCH的肺部灌注变化,并分析了这两种疾病中报道的PE型灌注缺陷以及潜在的肺部形态学变化。
共63名特发性或遗传性PAH患者(A组;n = 51)和PVOD/PCH患者(B组;n = 12)接受了DECT血管造影与形态学和灌注图像重建的研究。
A组(35/51;68.6%)和B组(6/12;50%)之间灌注异常的患者数量没有差异(P = 0.31),每个患者的平均灌注异常节段数也没有差异(A组:17.9 ± 4.9;B组:18.3 ± 4.1;P = 0.91)。最常见的发现是A组存在斑块状缺损(15/35;42.9%),B组存在灌注异常的不同关联(4/6;66.7%)。每位患者有PE型缺陷的节段的中位数百分比在B组明显高于A组(P = 0.041)。8名患者有两种类型的PE型缺陷(A组:5/51;9.8%;B组:3/12;25%),叠加在PH相关的肺部异常(7/8)或正常肺(1/8)。异常灌注患者的碘浓度明显较低(P<0.001),但组间无差异。
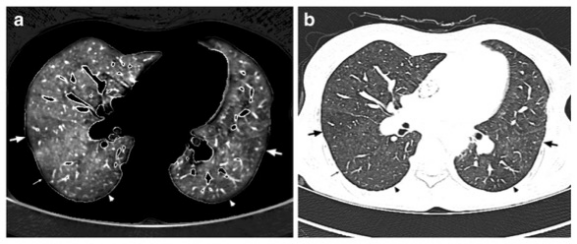
图 一个64岁的非吸烟特发性PAH女性患者的双能量CT图像。在上叶水平获得的1毫米层厚的灌注图像显示周边的小叶楔形灌注缺陷(箭头)。b 1毫米厚的CT横断面(肺部图像)与a所示相同,显示肺部衰减的镶嵌模式。箭头所指的是低衰减区域,叠加在a所示的小叶低灌注区域
本研究表明,DECT灌注异常在PVOD/PCH和特发性或遗传性PAH之间没有差异,但PVOD/PCH中具有PE型缺陷的节段比例较高,叠加了严重程度不同的PH相关的肺实质异常,这为进一步阐明其病理生理提供了思路及参考。
原文出处:
Briac Lefebvre,Maeva Kyheng,Jessica Giordano,et al.Dual-energy CT lung perfusion characteristics in pulmonary arterial hypertension (PAH) and pulmonary veno-occlusive disease and/or pulmonary capillary hemangiomatosis (PVOD/PCH): preliminary experience in 63 patients.DOI:10.1007/s00330-022-08577-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#毛细血管#
40
#动脉高压#
58
#PE#
38
#静脉#
0
#血管瘤#
57
#PAH#
43