Nat Commun:北大罗金才课题组等揭示血管内皮细胞分泌新机制
2017-03-08 佚名 生物帮
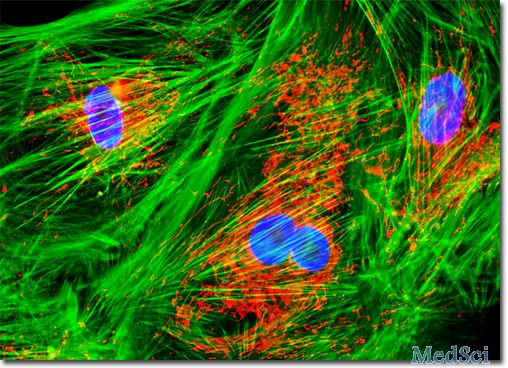
2017 年 3 月 3 日,国际学术权威刊物自然出版集团旗下子刊《Nature Communications》杂志在线发表了北京大学分子医学研究所罗金才教授研究组和中国科学院生物物理研究所李栋研究组合作的一篇研究论文,研究最新发现细胞黏附斑分子 Zyxin 是一个全新的 WP 小体分泌调控分子。论文题目为“Zyxin regulates endothelial von Willebrand fa
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#COMMUN#
28
#血管内皮细胞#
38
#罗金才#
40
#分泌#
36
#Nat#
32