Blood:αβT/B细胞敲除后进行HLA相合性造血干细胞移植(αβhaplo-HSCT)可有效治疗急性白血病
2018-10-23 MedSci MedSci原创
中心点:予以αβhaplo-HSCT治疗的急性白血病患儿发生急慢性GvHD的风险要低于进行非血缘供体移植的患儿的。αβhaplo-HSCT治疗后无GvHD、无复发的存活率要高于进行非血缘供体HSCT移植的患者。摘要:一直以来,来自于HLA匹配的血缘或无血缘供体(UD)的造血干细胞移植(HSCT)被用于治疗需要进行同种异体移植的急性白血病(AL)患儿。近期,一个单中心研究表明在αβT/B细胞敲除后进
予以αβhaplo-HSCT治疗的急性白血病患儿发生急慢性GvHD的风险要低于进行非血缘供体移植的患儿的。
αβhaplo-HSCT治疗后无GvHD、无复发的存活率要高于进行非血缘供体HSCT移植的患者。
摘要:
一直以来,来自于HLA匹配的血缘或无血缘供体(UD)的造血干细胞移植(HSCT)被用于治疗需要进行同种异体移植的急性白血病(AL)患儿。近期,一个单中心研究表明在αβT/B细胞敲除后进行HLA相合性HSCT(αβhaplo-HSCT)是有效的。
综上所述,本研究结果表明αβhaplo-HSCT适用于需要移植的AL患儿,特别是等位基因匹配的UD不可用时。
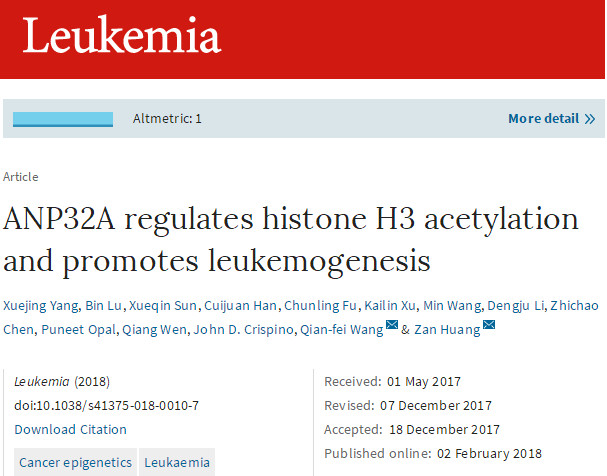
Alice Bertaina,et al. Unrelated donor vs HLA-haploidentical alpha/beta T-cell and B-cell depleted HSCT in children with acute leukemia. Blood 2018 :blood-2018-07-861575; doi: https://doi.org/10.1182/blood-2018-07-861575
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Haplo-HSCT#
34
#HSC#
35
#细胞移植#
28
#造血干细胞#
29
#B细胞#
34
#造血#
26
#HLA#
38
#APL#
0
#HSCT#
33
#有效治疗#
26