PHILIPS每日一例:支架辅助弹簧圈栓塞肾动脉瘤一例
2022-09-09 放射沙龙 放射沙龙
,RAA瘤颈宽度10 mm,若以单纯弹簧圈栓塞会增加远端分支动脉栓塞的风险。患者载瘤动脉为。
患者女,64岁。右腰背部不适1个月,行CTA检查发现右肾动脉主干远端一1.8 cm×2.8 em的囊状动脉瘤(图1)。
于局麻下行右肾动脉造影,见右肾动脉主干远端一1.8 em×2.8 cm的离心性动脉瘤,瘤体未明显累及远端分支,瘤颈宽度为10 mm(图2)。将一规格为5 mm×19 mm的Express球扩式支架(美国Boston Scientific)完全覆盖瘤颈释放。再送人Progreat导管(日本Terumo)从支架网孑L中穿入动脉瘤腔内,沿此导管陆续送人13枚微弹簧圈至瘤腔内进行栓塞(弹簧圈直径6mm 4枚、8 Rim 4枚、10 mm 5枚,图3)。
术后造影见瘤腔基本完全封闭,肾动脉主干及远端分支血流通畅;术后4 d无肾梗死(图4);术后1周患者肾功能无异常改变,无腰背痛等表现。
术后3个月及9个月随访无肾功能异常,CTA显示原。肾动脉瘤(renal artery aneurysm,RAA)腔基本封闭,瘤体缩小(图5),远端肾动脉各分支血流通畅,无肾梗死(图6)。
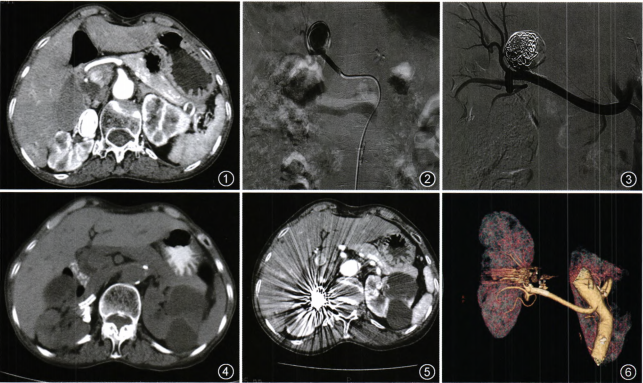
【图1术前增强CT见右肾动脉瘤
图2术中造影见右肾动脉主干宽颈动脉瘤
图3术中置人裸支架辅助弹簧圈栓塞
图4术后4 dCT见肾脏无梗死
图5术后3个月增强CT见瘤体缩小
图6术后9个月支架通畅,无肾梗死】
讨论RAA的处理主要包括:
随访、动脉瘤切除后肾动脉重建、腔内治疗和肾切除或部分肾切除术。传统外科手术操作复杂,需要充分暴露肾脏及肾动脉主干甚至分支,手术创伤和难度较大。腔内技术治疗RAA的方法主要包括经导管弹簧圈栓塞或覆膜支架腔内隔绝术、采用自体隐静脉覆盖的支架治疗。。窄瘤颈的囊状RAA可进行弹簧圈栓塞,对于宽颈瘤RAA可以使用覆膜支架腔内隔绝术治疗。
本例之所以选择支架辅助弹簧圈栓塞介入治疗,是根据其RAA的解剖学特点所决定。根据本例患者特点,RAA瘤颈宽度10 mm,若以单纯弹簧圈栓塞会增加远端分支动脉栓塞的风险。患者载瘤动脉为。肾动脉远端主干,且无明显扭曲,近端锚定区充分、远端锚定区较短,且分出肾上极与下极2个重要分支。若置入覆膜支架行腔内隔绝此宽颈动脉瘤,为保证远端锚定区充分,支架可能会覆盖并阻断远端肾下极分支动脉的血供。为保留所有分支动脉,不影响肾脏功能,
笔者最终选择用自膨式支架置人和微导管输送微弹簧圈栓塞的技术。这种方法可以防止微弹簧圈沿肾动脉血流进入远端动脉,保证远端所有分支的动脉血供。术后血管造影显示瘤腔基本封闭,。肾动脉主干至远端各分支血流通畅。术后3个月及9个月后随访无肾功能异常,CTA显示原RAA腔基本完全封闭,远端肾动脉各分支血流通畅,无肾梗死。通过对本例患者的治疗,笔者认为对于宽瘤颈的RAA,采用上述腔内技术对患者创伤小且更为安全。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#弹簧圈栓塞#
46
#iPS#
32
#肾动脉#
35