


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




患者10余年前出现间断腹痛,位于剑突下,程度较轻,为持续性隐痛,不伴放射,进食后疼痛可能缓解,持续数十分钟至数小时不等。患者无反酸、嗳气,无恶心、呕吐,无腹胀、腹泻。曾于外院行胃镜检查示“浅表性胃炎”,位于进一步治疗。2个月前开始出现左下腹痛,性质描述不清,程度中等,向左肋下及左腹股沟区放射,伴便意,大便性质正常,排便后腹痛可缓解。
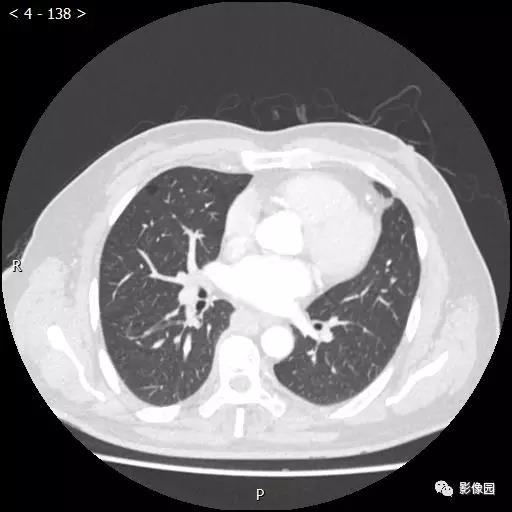
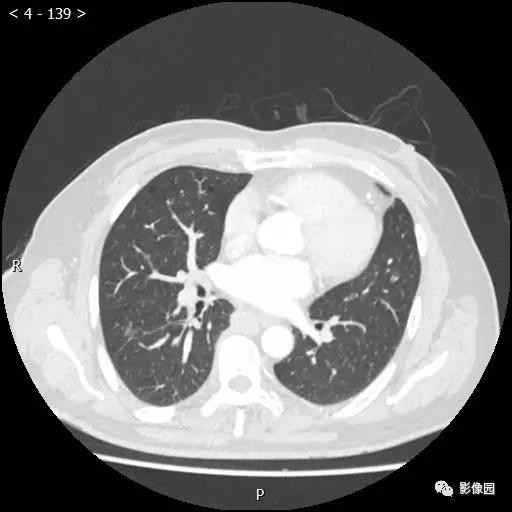
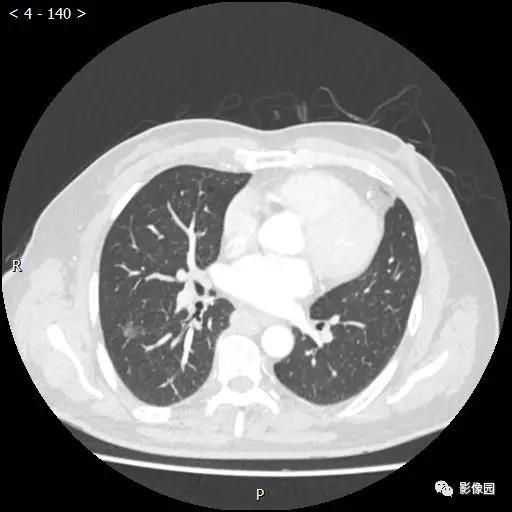
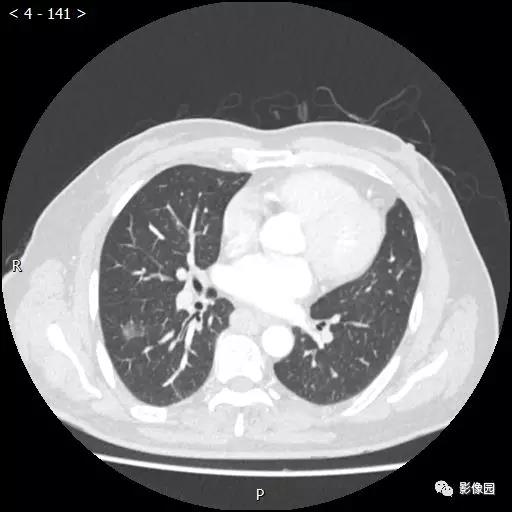
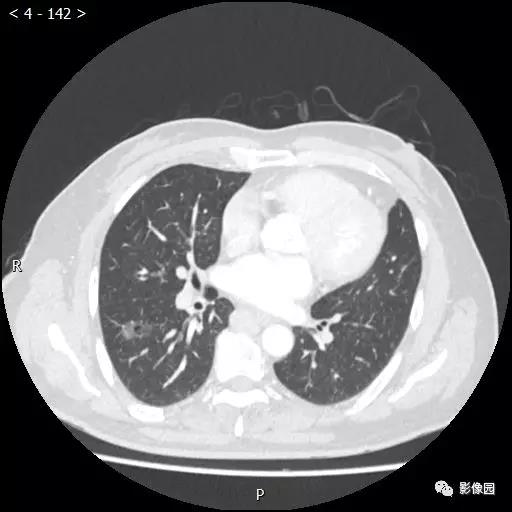
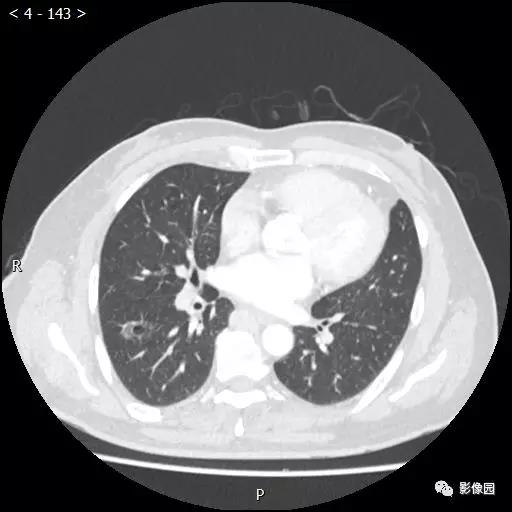
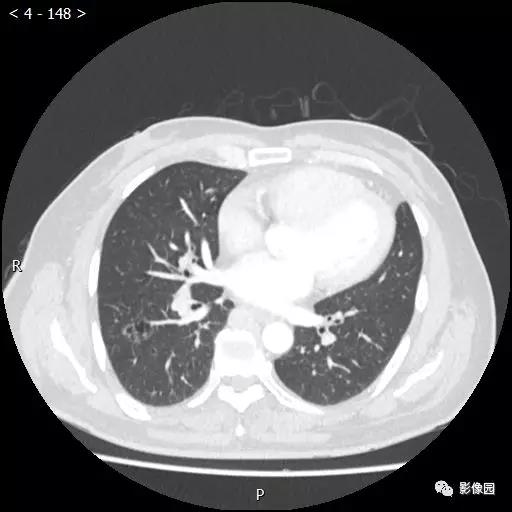
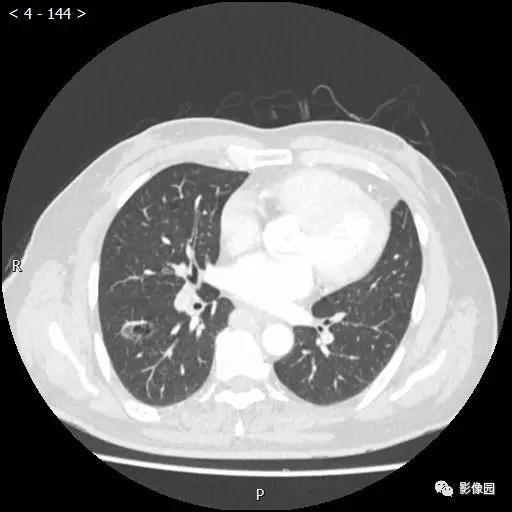
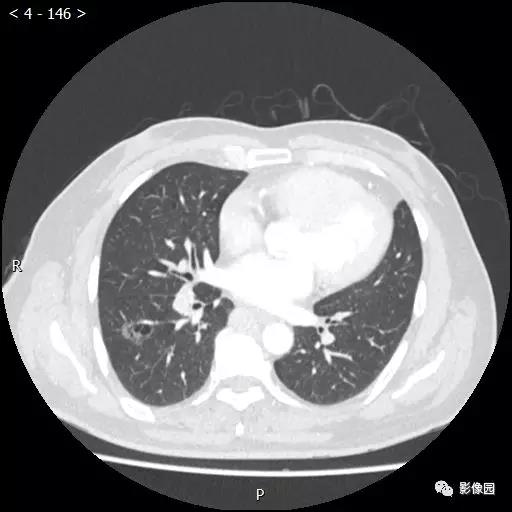
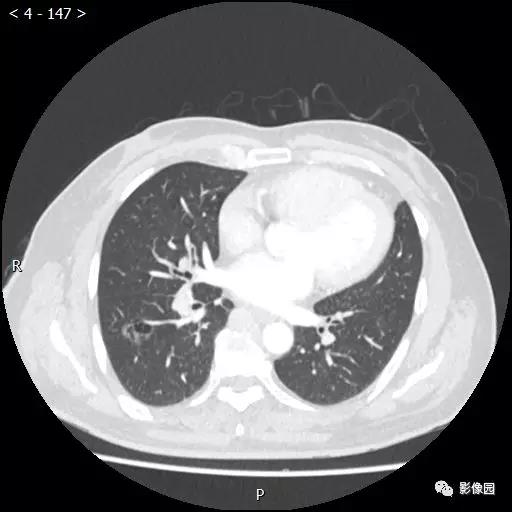
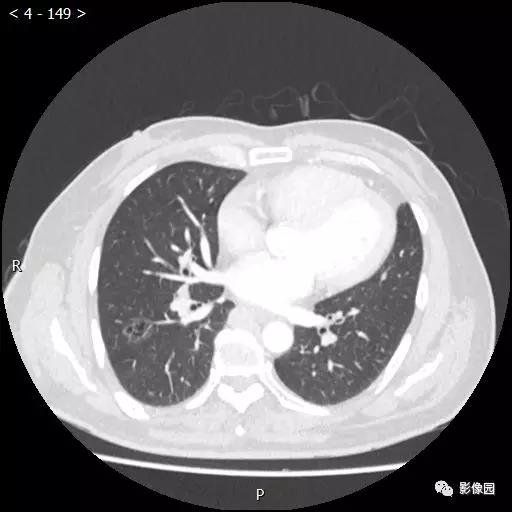
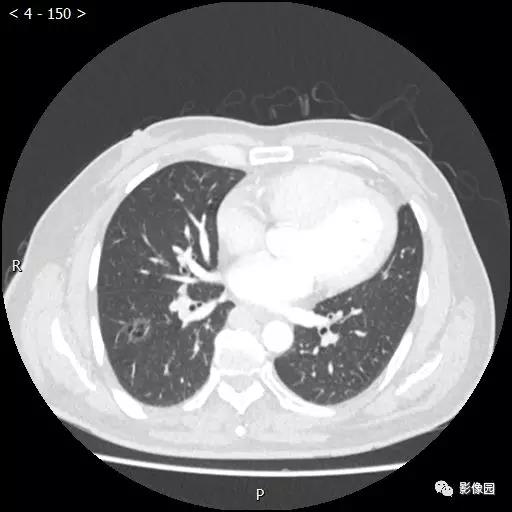
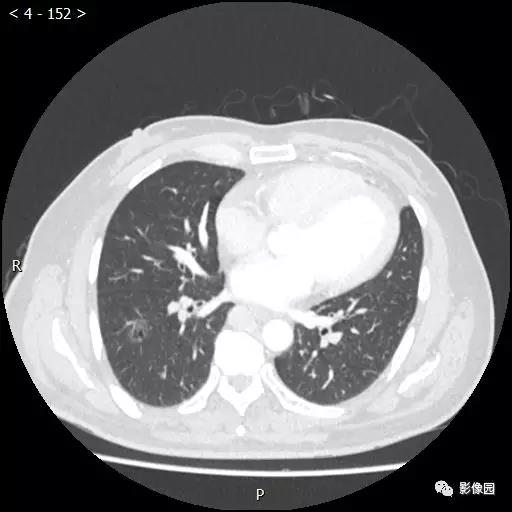
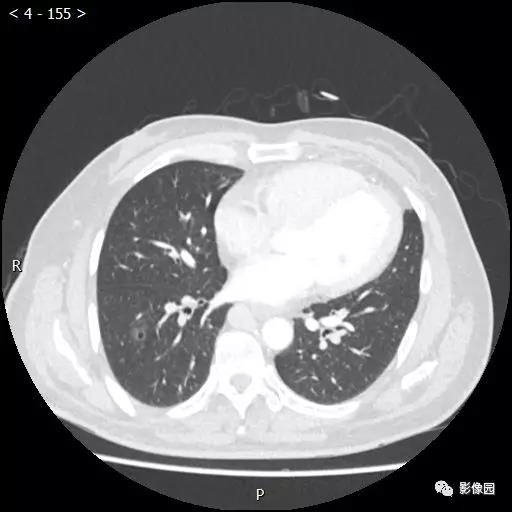
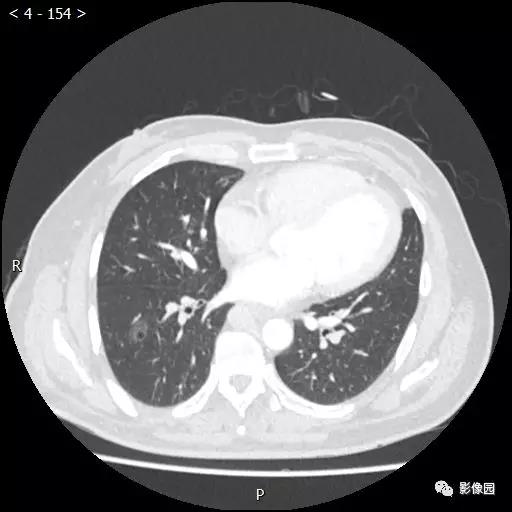
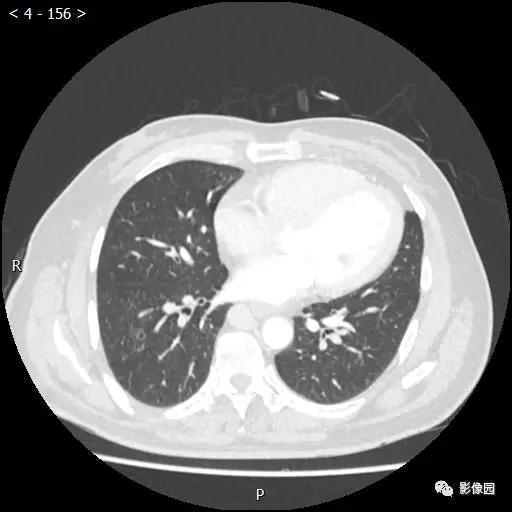
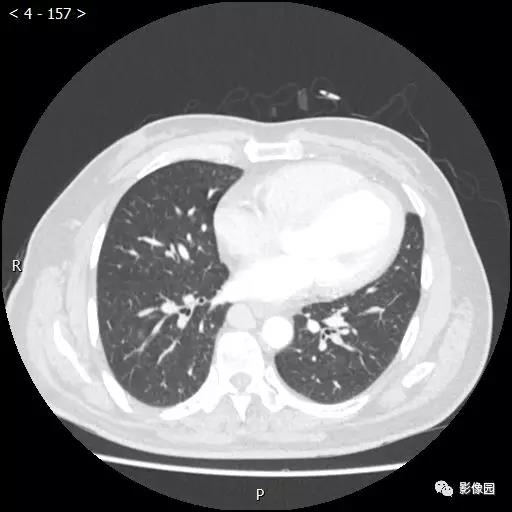
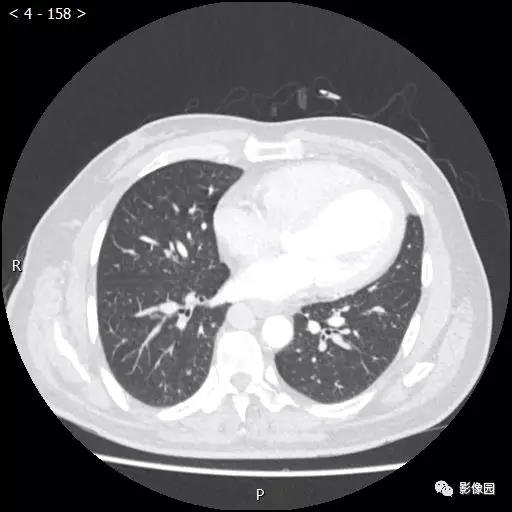
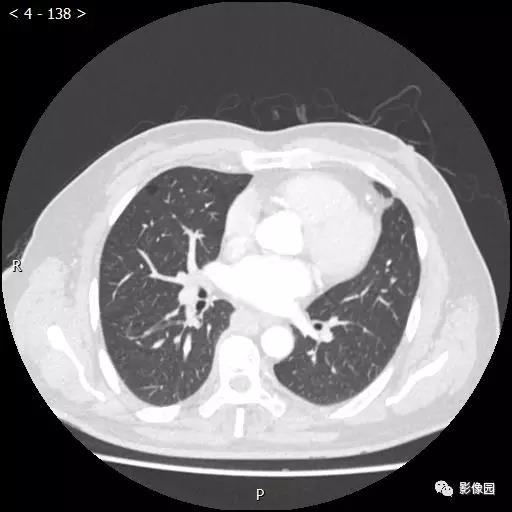
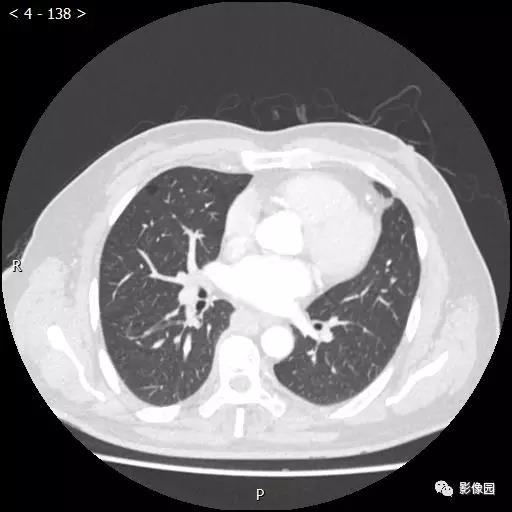
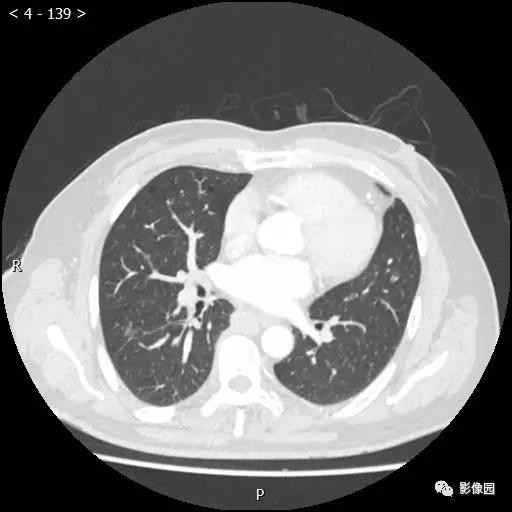
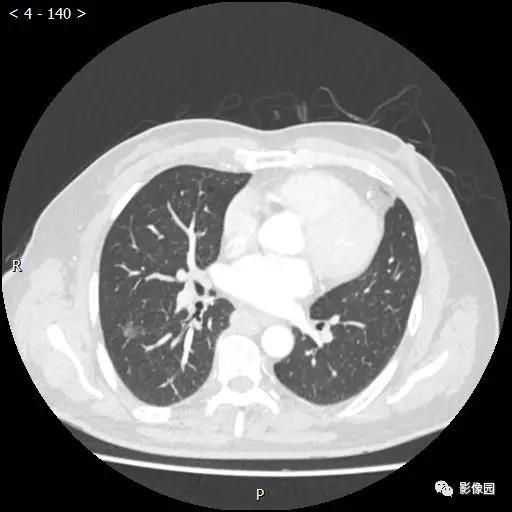
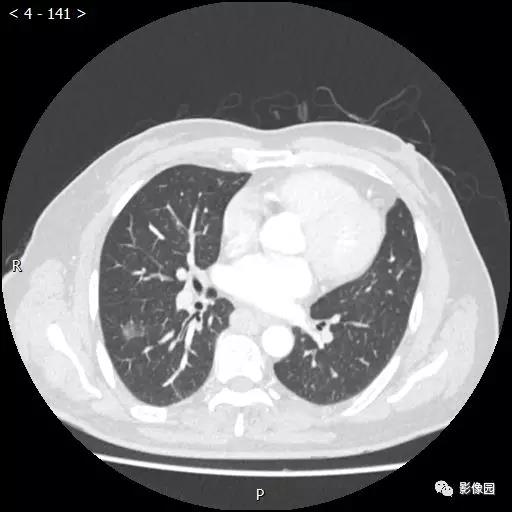
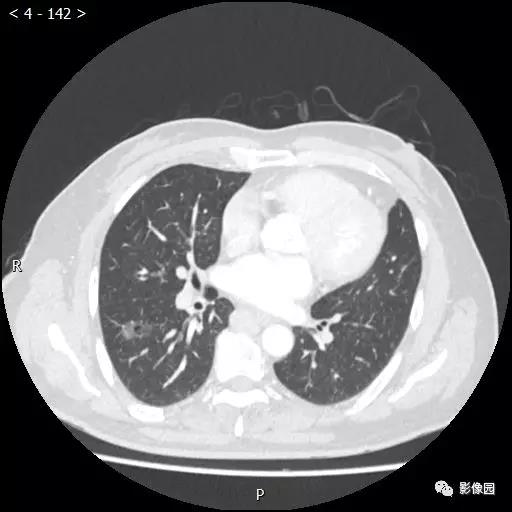
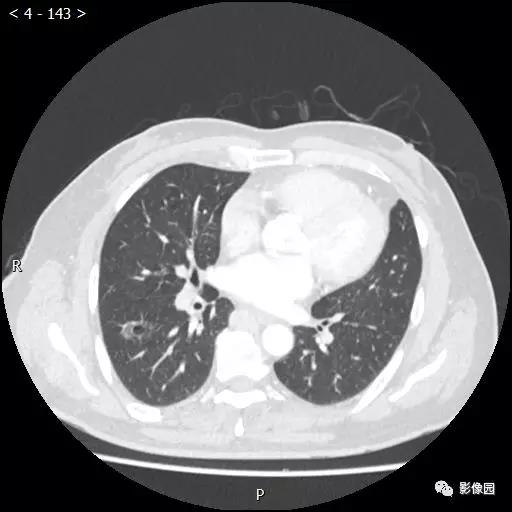
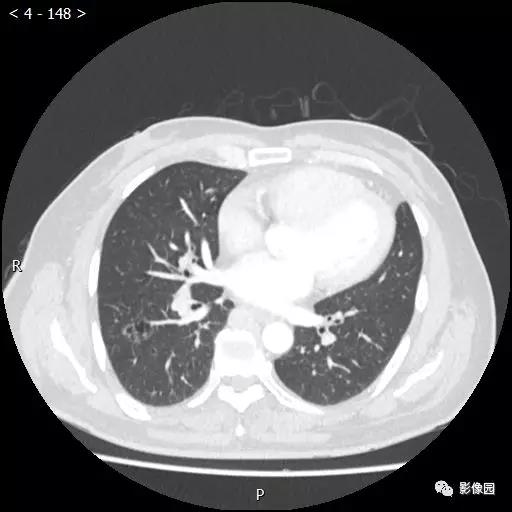
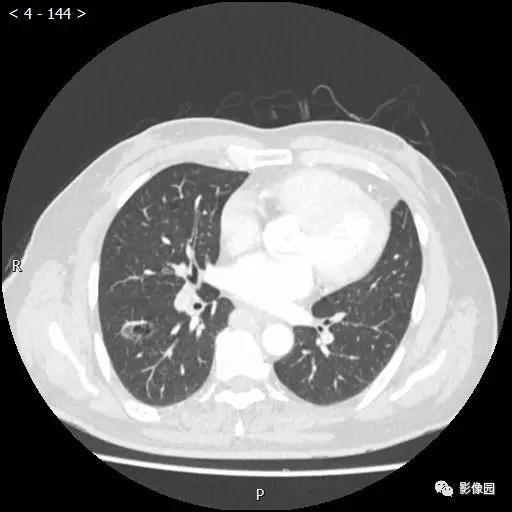
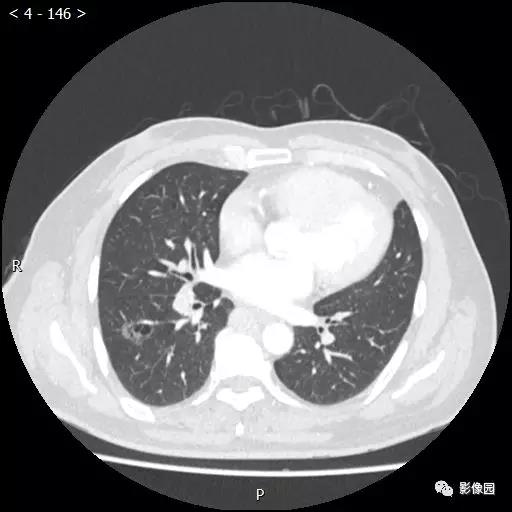
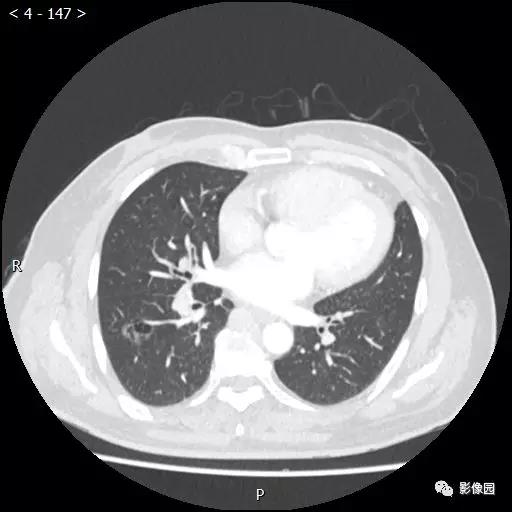
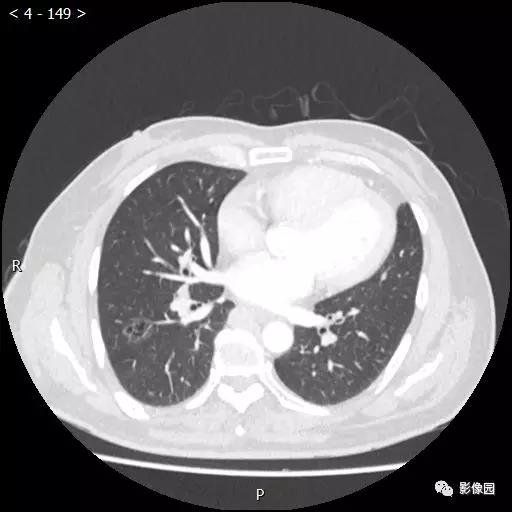
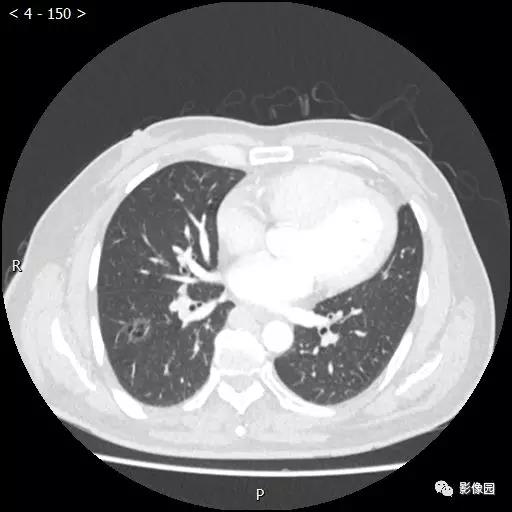
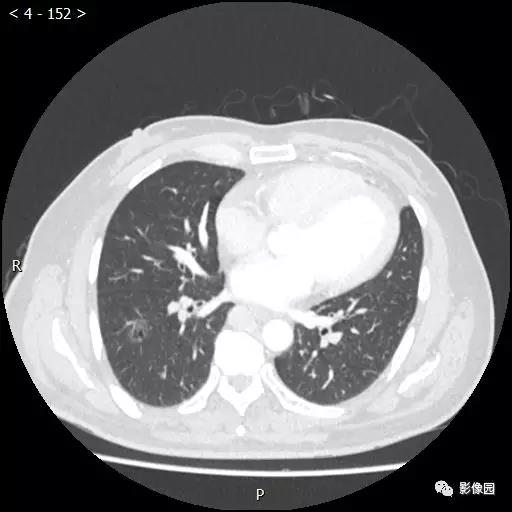
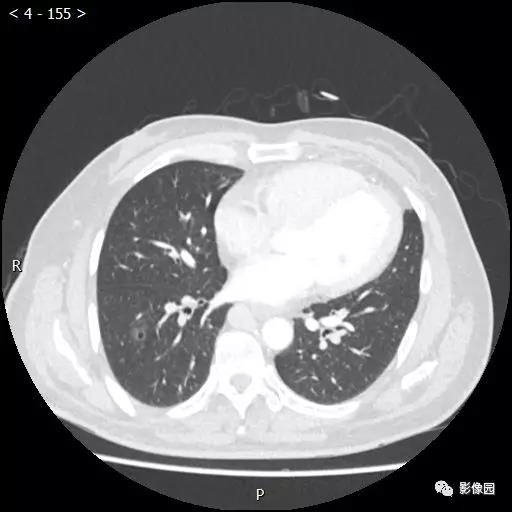
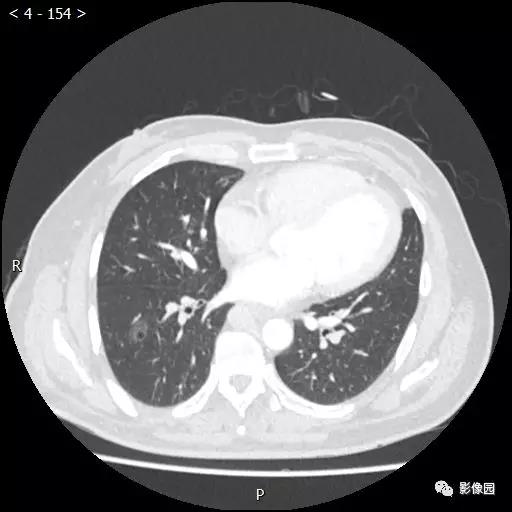
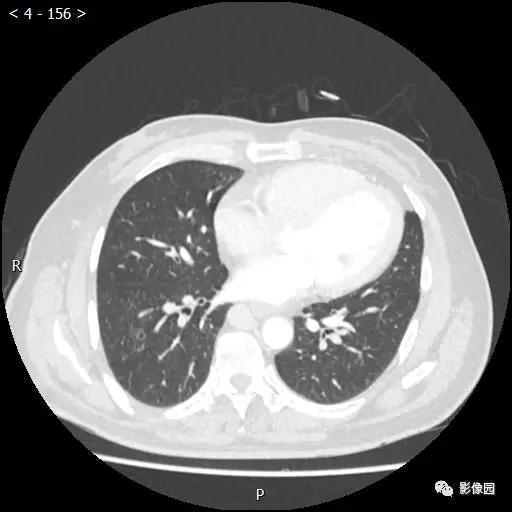
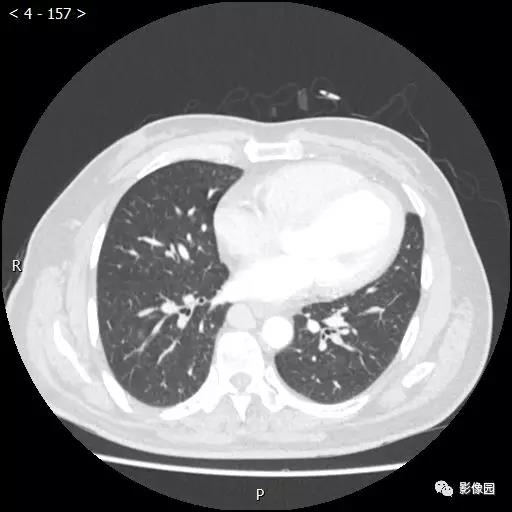
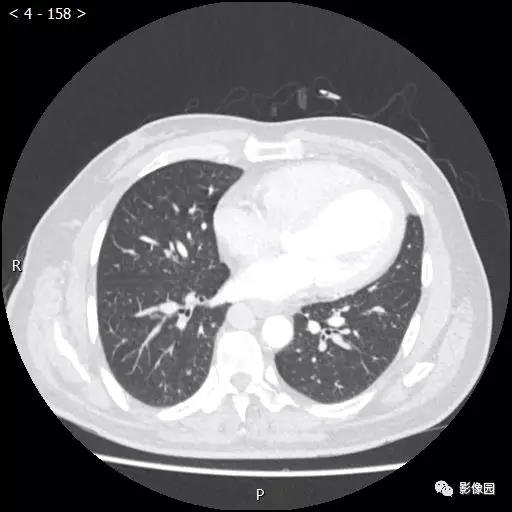
患者于10年前无明显诱因出现胸闷憋气、咳嗽、咳痰,为少量白痰,于外院就诊,行胸部CT检查提示“肺大泡,肺气肿”,未予治疗。半年前无明显诱因再次出现胸闷憋气,劳累后加重,爬1层楼即感胸闷憋气,夜间可平卧入睡,偶有咳嗽、咳痰,为少量白痰。
心衰伴保留型射血分数(HFpEF)被认为是老年疾病,青少年几乎不会患此疾病。本研究的目的旨在评估HFpEF患者的年龄、临床表现和预后之前的相关性。本研究纳入了3个大型HFpEF临床试验中左室射血分数≥45%的患者,并将患者根据年龄分为≤55 岁组(n=522),56-64岁组(n=1679),65-74岁组(n=3405),75-84岁组(n=2464)和≥85岁组(n=398)。比较了不同年龄段
患者,女,77岁,已绝经。自述左髋部疼痛1个月余,于本院门诊就诊,门诊查体+阅片示:左侧人工股骨头置换术后假体松动。拟收入本院行左侧人工全髋关节翻修术。患者左下肢血运、活动可,双下肢无水肿。既往于20年前因摔伤致左股骨颈骨折而行左侧人工股骨头置换术,否认高血压、糖尿病等慢性病史,否认其他手术史,否认其他重大外伤史,否认输血史,否认药物、食物及其他接触物过敏史,否认家族遗传病史。
患者女性73岁。现病史:绝经22年,22天前出现阴道间断流血时有时无鲜红色经妇科医生明确诊断为:子宫内膜癌。治疗方式:择期行广泛全子宫切除术。既往史:患者结肠癌术后30年,高血压病史10年,血压最高160/90mmHg,规律口服硝苯地平片控制,血压控制在130/70mmHg,糖尿病病史30年,近2年使用诺和灵30R早36U、晚34U皮下注射规律监测血糖FPG:9.3mmol/L,OGTT2h:10
随着年龄增长,心血管风险急剧增加,导致老年人群中几乎普遍存在基于风险的他汀类药物资格。为限制过度治疗,需确定真正低风险的老年人。JACC发表的一项研究旨在发现“负”风险标志物,以识别低短期风险的冠心病和心血管疾病老年人。


梅斯医学MedSci APP
医路相伴,成就大医
#突发胸痛#
28
#老年男性#
27
了解一下
75
了解一下
67
了解一下
65
了解一下
69