Stroke:中性粒细胞计数作为预测动脉瘤性蛛网膜下腔出血患者住院死亡率有前景的标志物
2021-06-28 MedSci原创 MedSci原创
在动脉瘤性蛛网膜下腔出血患者中,入院时较高的中性粒细胞计数与死亡率和医院获得性感染风险增加相关。中性粒细胞计数是一个简单、有用的标志物,对动脉瘤性蛛网膜下腔出血患者具有重要的预后价值。
全身炎症被认为是卒中的标志。近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在评估动脉瘤性蛛网膜下腔出血患者入院时使用血液的各种炎症因子的预后价值。

在这项针对动脉瘤性蛛网膜下腔出血患者的多中心观察性研究中,研究人员在受试者入院时收集其中性粒细胞、血小板和淋巴细胞的计数。
患者根据嗜中性粒细胞计数与倾向评分匹配进行分层,以尽量减少混淆。研究人员计算了院内死亡率和医院获得性感染的主要结局的调整后比值比和95%CI。
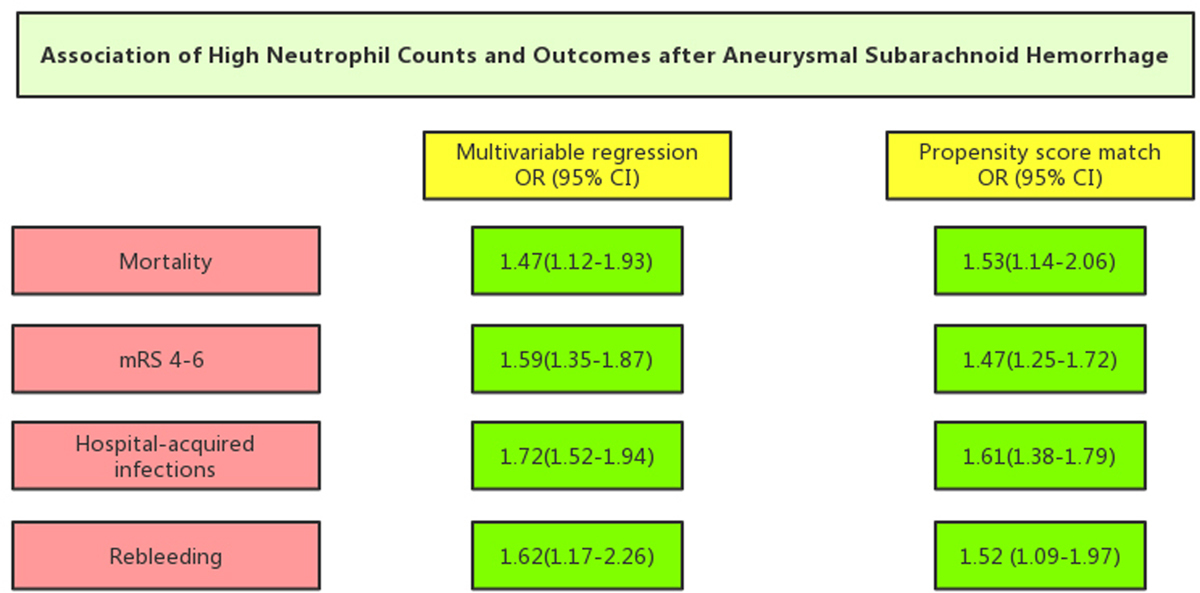
中性粒细胞计数与动脉瘤性蛛网膜下腔出血患者住院死亡率的关系
该研究共纳入了6041例患者,其中344例(5.7%)在医院内死亡。倾向评分匹配分析表明,与较低的中性粒细胞计数相比,较高的中性粒细胞计数与院内死亡率(比值比为1.53[95%CI为1.14-2.06])、医院获得性感染(比值比为1.61[95%CI为1.38-1.79])和迟发性神经缺血缺损(比值比为1.52[95%CI为1.09-1.97])相关。此外,在研究的所有炎症因子中,中性粒细胞计数与院内死亡率和医院获得性感染的关联程度最高。
由此可见,在动脉瘤性蛛网膜下腔出血患者中,入院时较高的中性粒细胞计数与死亡率和医院获得性感染风险增加相关。中性粒细胞计数是一个简单、有用的标志物,对动脉瘤性蛛网膜下腔出血患者具有重要的预后价值。
原始出处:
Yu Zhang.et al.Neutrophil Counts as Promising Marker for Predicting In-Hospital Mortality in Aneurysmal Subarachnoid Hemorrhage.stroke.2021.https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.034024
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#有前景#
30
#标志物#
0
#蛛网膜#
35
谢谢啦学习了
51
很不错👍简便的指标
83
已读,真是受益匪浅呀。
56
#中性粒细胞#
34
#动脉瘤性蛛网膜下腔出血#
40
#住院死亡率#
30
嗯
38